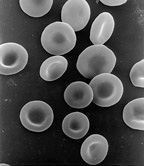
Photo from wikipedia
Topic Significance & Study Purpose/Background/Rationale Hematopoietic stem cell transplantation provides a curative alternative for malignant and non-malignant diagnoses, and Texas Children's Hospital's (TCH) Pediatric Bone Marrow Transplant (BMT) unit performs… Click to show full abstract
Topic Significance & Study Purpose/Background/Rationale Hematopoietic stem cell transplantation provides a curative alternative for malignant and non-malignant diagnoses, and Texas Children's Hospital's (TCH) Pediatric Bone Marrow Transplant (BMT) unit performs over 100 of these curative alternative transplants annually. Patients frequently experience clinical deterioration that results in increased morbidity and/or mortality. The purpose of this quality improvement project is to determine if the integration of blood pressure into the Pediatric Advanced Warning Score (PAWS) assessment would be an earlier predictor of initial clinical deterioration with patients in the conditioning, aplastic, engraftment and post discharge phases of treatment. Methods, Intervention, & Analysis TCH implemented the (PAWS) scoring system in 2009 as a validated and reliable scoring tool. The PAWS scoring system uses three categories of clinical indicators: behavior, cardiovascular status and respiratory status (Bell et al, 2013). BMT added blood pressure as a fourth clinical indicator for the PAWS assessment, validated the new scoring system through staff education and scoring patient scenarios and implemented in August 2018. When the early recognition algorithm triggered a score of four, the charge nurse, bedside nurse, attending physician and fellow completed a huddle to debrief on the current phase of treatment and abnormal clinical indicators to formulate a treatment plan based on the phase of transplant. Findings & Interpretation From October 2017 to July 2018, 70% (n=33) of BMT patients who required a Rapid Response Team (RRT) call were transferred to the Pediatric Intensive Care Unit (PICU). After project implementation, only 57% (n=14) of patients who required an RRT call were transferred to the PICU. Adding the blood pressure to the PAWS score decreased the initial recognition time to an average of 45 hours (range 17-62). Discussion & Implications The revised PAWS scoring tool and early recognition algorithm has demonstrated increased sensitivity to the identification of initial clinical deterioration, promoting better outcomes and decreased morbidity and mortality for our patients. We are continuing to monitor the BMT PAWS tool and patient outcomes.
Journal Title: Biology of Blood and Marrow Transplantation
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!