Photo from wikipedia
TOPIC: Chest Infections TYPE: Medical Student/Resident Case Reports INTRODUCTION: COVID-19 has awestruck physicians across the world with its atypical presentations. Often, pericarditis and myocarditis occur with viral infections in young… Click to show full abstract
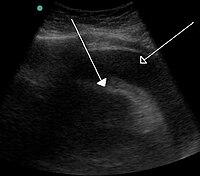
TOPIC: Chest Infections TYPE: Medical Student/Resident Case Reports INTRODUCTION: COVID-19 has awestruck physicians across the world with its atypical presentations. Often, pericarditis and myocarditis occur with viral infections in young adults. It is rare to see viral infections causing cardiac tamponade, which is a potentially fatal complication. Several cases of pericardial effusions and pre-tamponade physiology have been reported in elderly individuals with an extensive history of cardiac disease. Here, we describe the case of a previously healthy young adult who developed COVID-19 related cardiac tamponade without any preceding respiratory symptoms. CASE PRESENTATION: A 34-year-old female with a past medical history of hypothyroidism had tested positive for the SARS CoV-2 (Severe Acute Respiratory Distress Syndrome Coronavirus-2) one week prior to presentation. She presented with constant, central chest pain radiating to the back for 2 days. While being evaluated for hypotension, the patient broke into convulsions and was consequently intubated and mechanically ventilated. The patient's Brain natriuretic peptide (BNP) was elevated at 2,470 pg/mL (normal range: 0 – 450 pg/mL), and cardiac troponin was mildly elevated at 0.63 ng/mL. Initial electrocardiogram showed a low voltage strip with sinus tachycardia, and electrical alternans, suggestive of pericarditis(1). Computerized tomography (CT) of the chest with contrast revealed a small non-tappable pericardial effusion. CT head was negative. Over the course of a few hours, significant elevation of cardiac troponin to 5.18 ng/mL, and escalation in vasopressor requirements prompted us to obtain bedside echocardiography, which demonstrated a large pericardial effusion with pre-tamponade physiology. Emergent bedside pericardiocentesis was performed and 250cc of serous pericardial fluid was drained. A pericardial window was kept open to watch for re-accumulation. Post-procedural electrocardiogram had normal voltage, showed no electrical alternans and tachycardia had resolved. The patient was gradually weaned from vasopressor support and other supportive treatment. The pericardial drain was removed. An echocardiogram obtained at a 2-month follow-up showed a healthy heart with a normal ejection fraction. DISCUSSION: On initial evaluation, the differential diagnosis for convulsive syncope in a young patient with hypotension and COVID-19 were pulmonary embolism or a thromboembolic stroke. EKG findings and subsequent clinical course pointed towards a possible pericardial effusion. However, pericardial effusions are commonly idiopathic and only a smaller subset of cases stem from infectious disease. Viral pericarditis causes gradual accumulation of transudate leading to a pericardial effusion. Interestingly, in our patient cardiac tamponade was acute. CONCLUSIONS: This case underscores that an index of suspicion should be held for COVID-19 causing cardiac tamponade in young individuals and that prompt intervention is invaluable. REFERENCE #1: Eisenberg MJ, de Romeral LM, Heidenreich PA, Schiller NB, Evans GT Jr. The diagnosis of pericardial effusion and cardiac tamponade by 12-lead ECG. A technology assessment. Chest. 1996 Aug;110(2):318-24. doi: 10.1378/chest.110.2.318. PMID: 8697827. DISCLOSURES: No relevant relationships by Neha Panchagnula, source=Web Response
Journal Title: Chest
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!