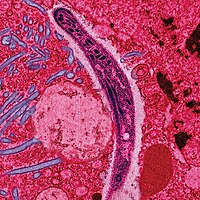
Photo from wikipedia
TOPIC: Chest Infections TYPE: Medical Student/Resident Case Reports INTRODUCTION: COVID-19 infection causes a wide range of clinical manifestations. Though the exact mechanism through which COVID-19 affects each system remains poorly… Click to show full abstract
TOPIC: Chest Infections TYPE: Medical Student/Resident Case Reports INTRODUCTION: COVID-19 infection causes a wide range of clinical manifestations. Though the exact mechanism through which COVID-19 affects each system remains poorly understood, the development of a cytokine-mediated systemic inflammatory response could explain the virus's multi-system impact. The effect of COVID-19 on the central nervous system is now well recognized. We present a case of COVID-19 with neuropsychiatric symptoms and accelerated worsening of chronic conditions. CASE PRESENTATION: A 63-year-old man with rheumatoid arthritis and depression presented with confusion, hallucinations, and extremity stiffness. Two months ago, he was admitted for COVID-19 pneumonia. Since then, he has experienced inability to walk, hallucinatory episodes, and insomnia. Episodes are recurrent with a return to baseline over 24 to 48 hours. He ultimately became non-ambulatory due to worsened joint deformities. On presentation, he was delirious with word repetition, inappropriate response to questions, and was profusely diaphoretic. Extremities were rigid and held in a semi-flexed position. Brisk reflexes were noted in lower extremities. There was no neck stiffness. Vitals and labs were stable. COVID-19 test negative. Non-contrast head CT showed subtle white matter changes. Brain MRI was unrevealing. EEG was mildly abnormal with diffuse background slowing, limited findings due to motion artifact. His symptoms considerably improved overnight, however, he continued to have episodes of disorientation and visual hallucinations with no time-of-day preference. He was managed with a low dose of Seroquel. Neurology diagnosed COVID-19 cerebritis with post-infection sequalae. Patient was referred for long-term physical therapy and rehabilitation. DISCUSSION: The COVID-19 pandemic created a paradigm shift in global health practices. Initially assumed to mainly affect the respiratory system with symptoms ranging from a mild flu-like illness to an ARDS phenotype, there is now literature evidence of disseminated disease. COVID-19 related encephalopathy occurs in 8.7% hospitalized patients, who are also more likely to have underlying medical co-morbidities. Other neurologic presentations include headache, generalized weakness, motor neuron disease, neuropathy, and seizures. Neuropsychiatric symptoms such as personality changes and hallucinations are commonly described in other coronavirus outbreaks. They are now seen in active COVID-19 infection and in the post infectious phase, termed Long-COVID syndrome. Also, this patient with underlying rheumatoid arthritis experienced accelerated disability, likely immune mediated. Timely evaluation, intervention and long-term rehabilitation can improve functional outcomes in these patients. CONCLUSIONS: Nervous system involvement in COVID-19 infection is a neurological diagnosis of exclusion in a patient who has tested positive for COVID-19 or has had known COVID-19 exposure. REFERENCE #1: Garg RK. Spectrum of Neurological Manifestations in Covid-19:A Review. Neurol India. 2020 May-Jun;68(3):560-572. doi:10.4103/0028-3886.289000. PMID:32643664 REFERENCE #2: Sheraton M, Deo N, Kashyap R, Surani S. A Review of Neurological Complications of COVID-19. Cureus. 2020;12(5):e8192. Published 2020 May 18. doi:10.7759/cureus.8192 REFERENCE #3: Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18-22. doi:10.1016/j.bbi.2020.03.031 DISCLOSURES: No relevant relationships by Ibimina Dagogo-Jack, source=Web Response No relevant relationships by Sukhmanjot Kaur, source=Web Response
Journal Title: Chest
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!