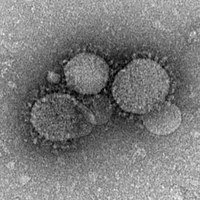
Photo from wikipedia
The risk of emerging infectious diseases such as Middle East respiratory syndrome coronavirus (MERS-CoV) [1] and Ebola epidemics is growing not only as the result of changes in demographic, anthropological,… Click to show full abstract
The risk of emerging infectious diseases such as Middle East respiratory syndrome coronavirus (MERS-CoV) [1] and Ebola epidemics is growing not only as the result of changes in demographic, anthropological, ecological and economic conditions but also because of increasing connectedness and speed of movement in the modernworld. In response to the risk of hospital transmissions to healthcare workers and other patients, maximum precautions in isolation wards aim to limit transmission. Infection due to MERS-CoV [2] was identified in 2012, and has been responsible for 1733 confirmed cases and 628 deaths to date [3]. In France, since 2012, 1524 patients were classified as possible cases, two were confirmed as MERS-CoV infection, of which one died [4]. Maximum precautions to avoid cross-transmission to healthcare workers may alter the management and care of other lifethreatening infectious diseases. It is of particular importance given the ratio between the number of cases of emerging infectious diseases and the number of ‘classical’ infections. A man in his sixties with possible MERS-CoV was admitted to our infectious diseases department at Bichat Claude Bernard Hospital in Paris in 2016. He lived in the United Arab Emirates and had returned to France for a holiday 5 days before admission. Fever had appeared 3 days earlier. He was initiated on amoxicillin by a general practitioner 2 days before. He was admitted to the emergency department for a persistent fever at 39.5 C with cough, shortness of breath and general weakness. His main medical and surgical history included an aortic prosthesis (Bentall surgery) with a mechanical aortic prosthesis, and a pacemaker implanted in 2002. The neutrophil count was 23 230/mm3, thrombocytes were low (97 000/mm3) and the C-reactive protein was elevated (386 mg/L). Chest X-ray was normal. The first hypothesis raised by the emergency department doctor was an infective endocarditis on the mechanical prosthesis. But the geographic provenance, the presence of fever and cough led to classification as a possible MERS-CoV, after case review with The ‘Institut national de Veille sanitaire’, according to the national recommendation. The patient was placed in the isolation ward 8 hours after admission (H8) through the emergency department. According to French guidelines for laboratory biosafety, initial processing of biological specimens should take place in a class II or class III biosafety cabinet. Only automatized tests could be collected and analysed. Other microbiological tests, such as blood
Journal Title: Clinical Microbiology and Infection
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!