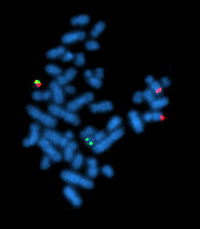
Photo from wikipedia
Myeloproliferative neoplasms (MPN) arise from the acquisition of genetic mutations in hematopoietic stem cells. Currently, patients receive treatment with cytotoxic agents, the JAK1/2 inhibitor, ruxolitinib, or pegylated forms of interferon… Click to show full abstract
Myeloproliferative neoplasms (MPN) arise from the acquisition of genetic mutations in hematopoietic stem cells. Currently, patients receive treatment with cytotoxic agents, the JAK1/2 inhibitor, ruxolitinib, or pegylated forms of interferon alpha (IFN-α). Ruxolitinib is highly effective in treating constitutional symptoms and splenomegaly, however, MPN patients rarely achieve molecular remissions or cure. In contrast, treatment with IFN-α can induce deep molecular remissions, as measured by allelic burden of the JAK2V617F driver-mutation, but treatment may be limited by side effects. There are now clinical trials underway investigating clinical synergy of ruxolitinib and IFN-α in MPN patients. However, the clinical benefits of this combination are currently unknown and deserve preclinical evaluation. We used a preclinical murine model of Jak2V617F-driven MPN to investigate the mechanisms of action of ruxolitinib and IFN-α, in particular, the effects on haematopoietic stem and progenitor cell populations. We demonstrate that ruxolitinib targets progenitor populations but does not deplete MPN disease initiating long-term hematopoietic stem cells (HSCs). Jak2V617F/+ long-term HSCs show hypersensitivity to IFN-α treatment through enhanced STAT1 signaling. Using a novel murine pegylated IFN-α, we show specific targeting of Jak2V617F/+ long-term HSCs in vivo. This was mediated through the preferential induction of reactive oxygen species and DNA damage in Jak2V617F/+ HSCs compared to wild-type HSCs after chronic treatment, offering a novel mechanistic explanation for IFN-α induced reduction of JAKV617F allelic burden in MPN patients. Interestingly, we demonstrate that the target cell specificity of ruxolitinib vs. IFN-α avoids potential antagonism in vivo, a finding with clinical relevance to future efforts to combine these two agents in patients with MPNs.
Journal Title: Experimental Hematology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!