Photo from wikipedia
hurdle to their future application. To circumvent this problatelet transfusion is an essential supportive therapy for atients with hemato-oncological disorders as many of them resent with thrombocytopenia and bleeding. Platelet… Click to show full abstract
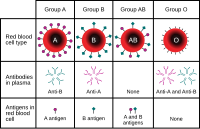
hurdle to their future application. To circumvent this problatelet transfusion is an essential supportive therapy for atients with hemato-oncological disorders as many of them resent with thrombocytopenia and bleeding. Platelet refracoriness, defined as the lack of adequate post-transfusion latelet count increment, remains a challenge in the manageent of platelet transfusion dependent patients. The majority f refractory cases have nonimmune causes and include infecion/sepsis, fever, splenomegaly, use of antibiotics and even torage conditions.1 Immune causes comprise ABO incompatbility, antibodies against class I human leukocyte antigens HLA) (mostly HLA-A and HLAB), and antibodies against uman platelet antigens (HPA). In hematology/oncology atients, platelet refractoriness has been reported in 7–34% f cases.2 The transfusion needs of patients with immune platelet efractoriness triggers a series of processes that include the dentification of the immune cause, the search for and notifiation of compatible donors in a genotyped donor bank, the onation of the actual blood product and finally its release and vailability for use. These are lengthy procedures, which are ostly and often unsuccessful. On the other hand, we have the efractory patient, bleeding or at imminent risk of bleeding, here urgency and agility are essential. These are two disonant situations attempting to converge on the same goal. n this regard, despite the few studies that rigorously assess leeding in patients requiring cross-matched platelet support, 3 he refractory state is associated with increased mortality. Thus, the development of technologies that aim to optiize the availability of the blood product as described by
Journal Title: Hematology, Transfusion and Cell Therapy
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!