Photo from wikipedia
OBJECTIVES The aim of this cross-sectional study was to investigate the pattern of antibiotic prescriptions for upper respiratory tract infections (URTIs) in children seen by primary care pediatricians (PCPs). METHODS… Click to show full abstract
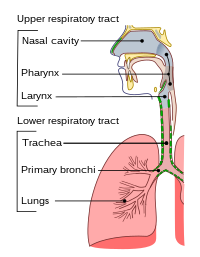
OBJECTIVES The aim of this cross-sectional study was to investigate the pattern of antibiotic prescriptions for upper respiratory tract infections (URTIs) in children seen by primary care pediatricians (PCPs). METHODS Data were collected from face-to-face interviews administered to a sample of parents of outpatient children aged 0-14 years in two regions in Southern Italy. To be eligible, children had to be diagnosed with sinusitis or pharyngotonsillitis or otitis media (AOM) or bronchitis or influenza or common cold. The presence of an indication of antibiotic therapy was evaluated according to national and international guidelines. RESULTS An antibiotic prescription was indicated in 57 (10.1%) of the sampled patients, of whom 33.3% did not receive an antibiotic prescription; among the 508 patients for whom an antibiotic prescription was not indicated, 27.4% received a prescription. Of all PCP consultations, 72% were appropriate (an antibiotic was prescribed when indicated and not prescribed when not indicated), whilst an antibiotic prescription not indicated by guidelines was given to 24.6% of the participants, and 3.4% of the sample did not receive an antibiotic prescription when indicated. The most frequently prescribed antibiotic was amoxicillin with clavulanic acid. A rapid microbiologic examination was performed in only 2 patients. CONCLUSIONS The study findings highlight a high rate of sub-optimal antibiotic therapeutic profile. Overprescription of antibiotic therapy and use of broad-spectrum molecules are widespread in children with URTIs. Antibiotic under-prescription, which may deprive pediatric patients of an effective treatment when indicated, also occurs.
Journal Title: International journal of antimicrobial agents
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!