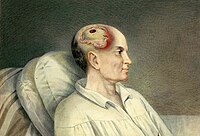
Photo from wikipedia
INTRODUCTION Computerized tomography (CT) imaging is a standard part of traumatic brain injury (TBI) evaluation but not all patients require it after mild head injury. Given the increasing incidence of… Click to show full abstract
INTRODUCTION Computerized tomography (CT) imaging is a standard part of traumatic brain injury (TBI) evaluation but not all patients require it after mild head injury. Given the increasing incidence of TBI in the United States, there is an urgent need to better characterize CT head imaging utilization in evaluating trauma patients, especially patients at low risk of requiring intervention, such as those presenting with a normal GCS. METHODS We analyzed the 2017-2019 National Trauma Databank using ICD-10 codes to identify patients who received a head CT. We used Abbreviated Injury Scale (AIS) scores to identify patients with a moderate to severe head injury defined as an AIS severity ≥ 3. Procedural TBI management was defined as having an intracranial monitor or operative decompression. We used a modified Poisson modeling to identify risk factors for a moderate/severe TBI and risk factors for undergoing procedural management among patients with head CT and GCS 15. RESULTS Of 2,850,036 patients, 1,502,039 (52.7%) had a head CT. Among patients who had a head CT, 1,078,093 patients (74.9%) had a GCS 15 on arrival. Of this group, only 16.6% (n = 176,431) had a moderate/severe head injury. For those with moderate/severe head injury, 6.0% (n = 10,544/176,431) of patients underwent procedural head injury management. Risk factors for undergoing procedural head injury management included: isolated head injury (RR 2.43, 95% CI 2.34, 2.53), male sex (RR 1.73, 95% CI 1.67, 1.80), age > 50 years (RR 1.39 95% CI 1.32, 1.47), falls (RR 1.28, 95% CI 1.22, 1.35), and the use of anti-coagulation (RR 1.16, 95% CI 1.11, 1.21). CONCLUSION Few patients had moderate/severe head injury when presenting with a GCS 15. However, patients ≥ 50 years, men, and those who suffered falls were at higher risk. Anti-coagulation use was not associated with moderate/severe head injury but did increase the risk of procedural TBI management. Given the cost and associated radiation, reducing CT utilization for younger patients while using a more liberal head CT strategy for high-risk patients may provide substantial patient value.
Journal Title: Injury
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!