Photo from wikipedia
STUDY OBJECTIVE To evaluate the clinical presentation and surgical outcome in patients with deep lateral pelvic endometriosis (dLPE). DESIGN A retrospective multicentric study (Canadian Task Force classification II-2). SETTING University… Click to show full abstract
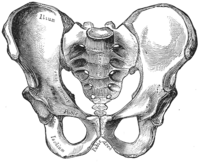
STUDY OBJECTIVE To evaluate the clinical presentation and surgical outcome in patients with deep lateral pelvic endometriosis (dLPE). DESIGN A retrospective multicentric study (Canadian Task Force classification II-2). SETTING University tertiary referral centers. PATIENTS One hundred forty-eight women with deep infiltrating endometriosis (DIE). INTERVENTIONS Laparoscopic excision of DIE. Disease distribution was classified as follows: central pelvic endometriosis (CPE) when DIE involved 1 of the following anatomic sites: cervix, vagina, uterosacral ligaments, rectum, bladder, or pelvic peritoneum; superficial lateral pelvic endometriosis when parametria, ureters, or hypogastric plexus were involved; and dLPE in the presence of sacral plexus and/or sciatic nerve infiltration. MEASUREMENTS AND MAIN RESULTS All patients showed CPE. LPE was detected in 116 cases (78.4%); among these, we observed dLPE in 41 patients (35.3%). dLPE occurred in 40% of women with CPE and in 72.7% of patients with hypogastric plexus involvement. Thirty women with dLPE (73.2%) received gastrointestinal or urologic resection in addition to gynecologic procedures compared with 40 patients (57.1%) without dLPE (p = .001). No differences were observed in terms of perioperative complications according to the presence of dLPE. According to univariate/multivariate analysis, chronic pelvic pain was the only predictor of dLPE (odds ratio = 3.041, p = .003). The median preoperative visual analog scale for dysmenorrhea (median = 8, range, 0-10) and dyspareunia (median = 5; range, 0-10) dropped to 0 after surgery. The median follow-up was 36 months (range, 6-66 months) with a recurrence rate of 8.8%. CONCLUSIONS dLPE is not a rare event in women with DIE. Complete laparoscopic removal of endometriosis seems to ensure benefit in terms of recurrence rate without increased surgical morbidities.
Journal Title: Journal of minimally invasive gynecology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!