Photo from wikipedia
PURPOSE To evaluate the impact of intentional coverage of accessory renal arteries (ARA) on renal outcomes after fenestrated-branched endovascular aortic repair (FB-EVAR) for pararenal aortic aneurysms or thoracoabdominal aortic aneurysm.… Click to show full abstract
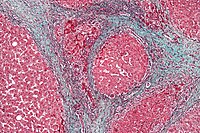
PURPOSE To evaluate the impact of intentional coverage of accessory renal arteries (ARA) on renal outcomes after fenestrated-branched endovascular aortic repair (FB-EVAR) for pararenal aortic aneurysms or thoracoabdominal aortic aneurysm. METHODS We analyzed the clinical data of 296 patients enrolled in a prospective non-randomized study to evaluate outcomes of FB-EVAR between 2013-2018. Patients with solitary kidneys, intraoperative loss of main renal arteries or pre-existing Stage V chronic kidney disease were excluded. Two groups were analyzed, patients with intentional ARA coverage and controls who had complete preservation. End-points included 30-day mortality, major adverse events (MAEs), acute kidney injury (AKI) defined by RIFLE criteria (Risk, Injury, Failure, Loss of kidney function, and End-stage renal disease), renal function deterioration (RFD) defined by >30% decline in baseline estimated glomerular filtration rate and presence of renal infarcts. RESULTS There were 254 patients (184 male, mean age 75±8 years old) included in the study, 56 (22%) with intentional ARA coverage and 198 controls, of which 16 had ARA preservation. ARA diameter was smaller in patients who had intentional coverage vs. preservation (2.7 ± 0.9 vs. 3.4 ± 0.2mm; p<.001). There was no difference in demographics, cardiovascular risk factors and aneurysm extent. All ARAs intended to be incorporate were successfully stented. Patients with ARA coverage had a higher frequency of kidney infarction (75% vs. 25%; p<.001). There were two (1%) deaths within 30-days, both among controls. Patients with ARA coverage had more MAEs (32% vs. 19%; p=.04) due higher incidence of AKI (21% vs. 9%; p=.02). None of the 16 patients who had ARA preservation developed AKI. At 3-years, freedom from RFD was lower for patients who had ARA coverage compared with controls (55 ± 9 vs. 76 ± 5%; log-rank=.02). By multivariate analysis, predictors of AKI were ARA coverage (OR, 2.8; 95% CI, 1.2 - 6.2; p=.01) and estimated blood loss > 1L (OR, 3.8; 95% CI, 1.2 - 12.3; p=.03). Post-operative AKI (HR, 4.4; 95% CI, 2.4 - 8.1; p<.001), renal reintervention for stenosis (HR, 3.2; 95% CI, 1.6-6.7; p=.002), aneurysm diameter (HR, 1.04; 95% CI, 1.02 - 1.06; p<.001) and ARA coverage (HR, 2.0; 95% CI, 2.4 - 8.1; p=.02) were predictors of RFD. CONCLUSION Intentional ARA coverage during FB-EVAR was associated with a threefold increase in AKI and with lower freedom from RFD. Factors associated with RFD included post-operative AKI, renal reinterventions for stenosis and ARA coverage. Incorporation of ARAs during FB-EVAR, when technically feasible, helps decrease risk of AKI and RFD.
Journal Title: Journal of vascular surgery
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!