Photo from wikipedia
Pyridoxine dependent epilepsy (PDE) (OMIM#266100) is a neonatal form of epilepsy, caused by dysfunction of the enzyme α-aminoadipic semialdehyde dehydrogenase (ALDH7A1 or Antiquitin). This enzyme converts α-aminoadipic semialdehyde (α-AASA) into… Click to show full abstract
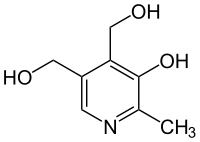
Pyridoxine dependent epilepsy (PDE) (OMIM#266100) is a neonatal form of epilepsy, caused by dysfunction of the enzyme α-aminoadipic semialdehyde dehydrogenase (ALDH7A1 or Antiquitin). This enzyme converts α-aminoadipic semialdehyde (α-AASA) into α-aminoadipate (AAA), a critical step in the lysine metabolism of the brain. ALDH7A1 dysfunction causes an accumulation of α-AASA and δ1-piperideine-6-carboxylic acid (P6C), which are in equilibrium with each other. P6C binds and inactivates pyridoxal 5'-phosphate (PLP), the active form of pyridoxine. Individuals affected by ALDH7A1 deficiency show pre-natal and post-natal seizures, which respond to oral pyridoxine but not to other pediatric anti-epileptic drugs. We discovered a novel missense mutation (c.566G > A, p.Gly189Glu) in homozygous state residing in the NAD+ binding domain coding region of exon 6 and affecting an highly conserved amino acid residue. The seizures stopped under post-natal pyridoxine therapy, nevertheless a longer follow-up is needed to evaluate the intellectual development of the child, who is additionally treated with oral l-arginine since the 13th month of life. Developmental delay with or without structural cortex abnormalities were reported in several patients. A brain MRI scan revealed hyperintense white matter in the right cerebellum compatible with cerebellar gliosis. Taken together, our studies enlarge the group of missense pathogenic mutations of ALDH7A1 gene and reveal a novel cerebellar finding within the PDE patients cohort.
Journal Title: Molecular and cellular probes
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!