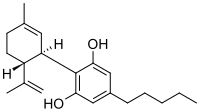
Photo from wikipedia
Cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC) are the most represented phytocannabinoids in Cannabis sativa plants. However, CBD may present with a different activity compared with the psychotomimetic THC. Most typically, CBD… Click to show full abstract
Cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC) are the most represented phytocannabinoids in Cannabis sativa plants. However, CBD may present with a different activity compared with the psychotomimetic THC. Most typically, CBD is reported to be used in some medical conditions, including chronic pain. Conversely, the main aim of this systematic review is to assess and summarise the available body of evidence relating to both efficacy and safety of CBD as a treatment for psychiatric disorders, alone and/or in combination with other treatments. Eligible studies included randomized controlled trials (RCT) assessing the effect of CBD in a range of psychopathological conditions, such as substance use; psychosis, anxiety, mood disturbances, and other psychiatric (e.g., cognitive impairment; sleep; personality; eating; obsessive-compulsive; post-traumatic stress/PTSD; dissociative; and somatic) disorders. For data gathering purposes, the PRISMA guidelines were followed. The initial search strategy identified some n = 1301 papers; n = 190 studies were included after the abstract's screening and n = 27 articles met the inclusion criteria. There is currently limited evidence regarding the safety and efficacy of CBD for the treatment of psychiatric disorders. However, available trials reported potential therapeutic effects for specific psychopathological conditions, such as substance use disorders, chronic psychosis, and anxiety. Further large-scale RCTs are required to better evaluate the efficacy of CBD in both acute and chronic illnesses, special categories, as well as to exclude any possible abuse liability.
Journal Title: Neurotoxicology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!