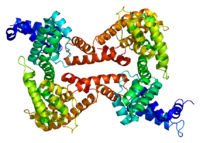
Photo from wikipedia
BACKGROUND Vitamin D deficiency represents a major health problem in general population, especially for its association with cardiovascular disorders and thrombotic risk, even in patients on dual antiplatelet therapy (DAPT).… Click to show full abstract
BACKGROUND Vitamin D deficiency represents a major health problem in general population, especially for its association with cardiovascular disorders and thrombotic risk, even in patients on dual antiplatelet therapy (DAPT). Vitamin D Binding Protein (VDBP) is the main transporter of vitamin D in the bloodstream and genetic polymorphisms of this protein have been shown to account for a significant variability of vitamin D levels and its systemic effects. Contrasting data have linked the rs7041 T→G substitution with cardiovascular disease. However, no study has so far addressed the role of rs7041 polymorphism on platelet reactivity in patients on DAPT, that was the aim of the present study. METHODS Patients treated with DAPT (ASA and clopidogrel or ticagrelor) for an ACS or elective PCI were scheduled for platelet function assessment at 30-90days post-discharge. Platelet function was assessed by Multiplate® (Roche Diagnostics AG), and VDBP genetic status by polymerase chain reaction and restriction fragment length polymorphism technique. Fasting samples were obtained for main chemistry parameters and vitamin D levels assessment. RESULTS We included 400 patients, 187 (46.8%) receiving clopidogrel and 213 (53.2%) ticagrelor. The genetic polymorphism rs7041 (T→G) was observed in 318 patients, (79.5%), in 38.7% of them in homozygosis. Main clinical and chemistry features did not significantly differ according to genetic status, but for a higher rate of ACE-inhibitors and beta-blockers use among the carriers of the G allele (p=0.04 and p=0.01, respectively). VDBP genetic status did not affect the rate of HRPR with ADP-antagonists (25.6% vs 24.6% vs 28.5%, p=0.59; adjusted OR[95%CI]=0.94[0.52-1.7], p=0.83 for T/G patients; adjusted OR[95%CI]=1.14[0.6-2.2], p=0.67 for G homozygotes). However, the rate of HRPR with ADP-antagonists was influenced by severe hypovitaminosis D (< 10ng/ml) only in patients carrying the G allele, especially in homozygosis (T/T: 25.9% vs 26.1%, p=0.99; G carriers: 22.1% vs 35.3%, p=0.02, pinteraction=0.019; adjusted OR[95%CI]=1.93[1.11-3.34], p=0.02 for G carriers). CONCLUSION The present study shows that rs7041 polymorphism of Vitamin D Binding Protein does not affect platelet reactivity or the rate of HRPR among patients receiving DAPT. However the carriage of the G allele could condition the impact of hypovitaminosis D on the response to antiplatelet agents, increasing the occurrence of HRPR especially in homozygotes, thus suggesting a more significant role of vitamin D deficiency among these patients.
Journal Title: Vascular pharmacology
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!