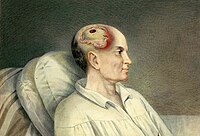
Photo from wikipedia
OBJECTIVE According to level 2 evidence, earlier evacuation of acute subdural or epidural hematomas necessitating surgery is associated with better outcome. Hence, guidelines recommend performing these procedures immediately. Literature on… Click to show full abstract
OBJECTIVE According to level 2 evidence, earlier evacuation of acute subdural or epidural hematomas necessitating surgery is associated with better outcome. Hence, guidelines recommend performing these procedures immediately. Literature on the extent and causes of prehospital and intrahospital intervals in patients with trauma requiring emergent craniotomies is almost completely lacking. Studies delineating and refining the interval before thrombolytic agent administration in ischemic stroke have dramatically reduced the door-to-needle time. A similar exercise for trauma-to-decompression time might result in comparable reductions. We aim to map intervals in emergent trauma craniotomies in our level 1 trauma center, screen for associated factors, and propose possible ways to reduce these intervals. METHODS We analyzed patients who were primarily referred (1R; n = 45) and secondarily referred (after computed tomography imaging in a community hospital [2R; n = 22]) to our emergency department (ED) and underwent emergent trauma craniotomies between 2010 and 2016. RESULTS Median prehospital interval (between emergency call and arrival at the ED) was 42 minutes for 1R patients. Median intrahospital interval (between initial ED arrival and skin incision [SI]) was 140 minutes and 268 minutes for 1R and 2R patients, respectively. In 1R patients, ED-SI interval was positively correlated with Glasgow Coma Scale score (ρ=.49; P < 0.001), but not with age, time of ED arrival, or extended Glasgow Outcome Scale score at 6 months. Based on outlier analysis, we propose prehospital and intrahospital measures to improve performance. CONCLUSIONS This is the first report on emergency call-SI interval in emergent trauma craniotomy, with a median of 174 minutes and >297 minutes for 1R and 2R patients, respectively, in our center.
Journal Title: World neurosurgery
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!