Photo from wikipedia
BACKGROUND As the prevalence of spinal fusion surgery has increased, reliable and safe bone graft substitutes have been developed in response. Biocompatible osteoconductive polymer (BOP) has been used as bone… Click to show full abstract
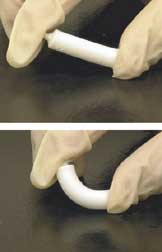
BACKGROUND As the prevalence of spinal fusion surgery has increased, reliable and safe bone graft substitutes have been developed in response. Biocompatible osteoconductive polymer (BOP) has been used as bone graft alternative for spine surgery. We present a case of cervical myelopathy due to extrusion of BOP 23 years after surgery and discuss the pathophysiology in terms of spinal fusion. CASE DESCRIPTION A 65 year old male patient presented with a 3 month history of cervical myelopathic symptoms. Twenty-three years ago, the patient had undergone cervical surgery for a C6-7 herniated disc using BOP. Imaging studies of the cervical spine showed cord compression due to extruded BOP at C6-7. He underwent corpectomy of the C7 vertebral body and removal of the BOP for the neural decompression, combined with interbody fusion using an iliac bone graft and plate fixation. During the operation, crumbly fibers of the BOP were easily removed. His myelopathic symptoms improved immediately after surgery. Post-operative magnetic resonance imaging also showed successful decompression of the spinal cord. Histologically, a foreign body reaction and bony degeneration were founded around the synthetic fibers of the BOP. CONCLUSIONS Spine surgeons should recognize the pathophysiology of the BOP used for spine fusion surgery. Although the BOP is not currently used for spinal surgery, patients undergoing previous surgery using the BOP can present with related complications. Revision surgery is recommended to remove the unincorporated BOP and achieve solid spine fusion.
Journal Title: World neurosurgery
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!