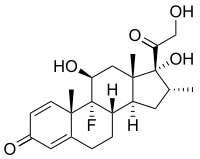
Photo from wikipedia
Corticosteroids are used in the treatment of many diseases; however, they also induce various side effects. Dexamethasone is one of the most potent corticosteroids, and it has been reported to… Click to show full abstract
Corticosteroids are used in the treatment of many diseases; however, they also induce various side effects. Dexamethasone is one of the most potent corticosteroids, and it has been reported to induce the side effect of impaired salivary gland function. This study aimed to evaluate the effects of dexamethasone on mouse submandibular gland function to gain insight into the mechanism of dexamethasone-induced salivary hypofunction. The muscarinic agonist carbachol (CCh) induced salivary secretion and was not affected by short-term dexamethasone treatment but was decreased following long-term dexamethasone administration. The expression levels of the membrane proteins Na+-K+-2Cl− cotransporter, transmembrane member 16A, and aquaporin 5 were comparable between the control and long-term dexamethasone treatment groups. The CCh-induced increase in calcium concentration was significantly lower in the presence of extracellular Ca2+ in the long-term dexamethasone treatment group compared to that in the control group. Furthermore, CCh-induced salivation in the absence of extracellular Ca2+ and Ca2+ ionophore A23187-induced salivation was comparable between the control and long-term dexamethasone treatment groups. Moreover, salivation induced by the Ca2+-ATPase inhibitor thapsigargin was diminished in the long-term dexamethasone treatment group. In summary, these results demonstrate that short-term dexamethasone treatment did not impair salivary gland function, whereas long-term dexamethasone treatment diminished store-operated Ca2+ entry, resulting in hyposalivation in mouse submandibular glands.Corticosteroids: revealing the mechanism of drug-induced dry mouthLong-term corticosteroid use causes dry mouth by inhibiting calcium movement into salivary gland cells. Corticosteroid use is associated with multiple systemic side effects including salivary inhibition, prompting Yusuke Kondo and a research team from Japan’s Kyushu Dental University to elucidate the reasons why. Submandibular glands taken from mice after six weeks’ treatment with the corticosteroid dexamethasone produced significantly less saliva in ten minutes than a group given just one week’s treatment, or no treatment at all. Further investigation revealed that long-term dexamethasone treatment inhibited the ability of salivary gland cells, known as acinar cells, to transport calcium ions from the exterior to the interior of the cells—an essential mechanism enabling salivation. The study improves our understanding of corticosteroid-induced dry mouth and reveals potential pharmacological targets to enable treatment.
Journal Title: International Journal of Oral Science
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!