Photo from wikipedia
Recent clinical trial and population-based registry reports claimed survival of persons with chronic phase chronic myeloid leukaemia (CML) receiving tyrosine kinaseinhibitor (TKI) therapy, especially those achieving a complete cytogenetic response… Click to show full abstract
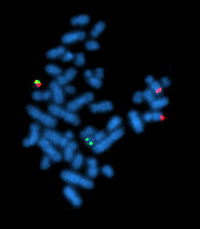
Recent clinical trial and population-based registry reports claimed survival of persons with chronic phase chronic myeloid leukaemia (CML) receiving tyrosine kinaseinhibitor (TKI) therapy, especially those achieving a complete cytogenetic response (CCyR; no detectable Ph-chromosome) and/or a sustained deep molecular responses (DMR; >4 or 4.5 log reduction in BCRABL1 transcripts), is similar to that of ageand sex-matched controls [1–4]. Is this so? Although there is a high response rate to TKItherapy, some responders relapse and a few develop blast transformation. Others become intolerant of and/or noncompliant with TKI-therapy whilst still others discontinue TKI-therapy because of fiscal considerations or adverse events [5]; 2nd and 3rd generation TKIs used in persons responding inadequately to 1st generation TKI-therapy associate with some adverse events which are lifethreating [6]. TKI-therapy can be successfully stopped in only about 20% of persons with CML (reviewed in [7, 8]). Lastly, it is rather unlikely TKI-therapy eliminates CML stem cells in anyone (reviewed in [9]). To determine if the most people with CML really have a normal life expectancy we used our software SEERaBomb [10] to interrogate the US Surveillance and Epidemiology End Results (SEER) dataset. To observed deaths (O) we fitted expected numbers m equal to a modelled rate multiplied by deaths expected (E) if subject follow-up time intervals were randomly selected from the US population for the same age, sex and calendar year. Poisson regression yielded an excellent fit to relative risks (RR) of death (O/E vs. m/E in Fig. 1a). Relative to survival plots of the same data (Fig. 1b), advantages of RR include a standard reference line (RR= 1) indicating how close we are to cure. Fitting m 1⁄4 1þ k1e1 k1t þ k2e2 k2t þ c3 E to O, in the limit of large times t since diagnosis, c3 indicates persons with CML in the US have a 2.38-fold (95% confidence interval; 1.70, 3.07; P < 0.0001) higher risk of death than controls. Although the SEER dataset includes a small proportion of subjects with acute phase CML and with Phchromosome-negative CML, this does not explain our finding of worse survival of persons with CML. Nor do differences in healthcare systems as life expectancy in the countries studied are similar. Of possible explanations for the discordance between our conclusion and those of clinical trials and population-based registries, the most likely is access to, compliance with and monitoring of TKI-therapy. A real world US study of people with CML reported infrequent molecular monitoring of response to TKI-therapy [11]. We found a similar deficiency in molecular monitoring in China [12]. There also may be other explanations such as lack or insufficient access to healthcare. In a US population-based study, persons with >85% access to TKIs via Medicare had comparable survival to ageand sex-matched controls [4], suggesting our finding of decreased survival comes from those on Medicare with <85% access to TKI and/or other, likely under-insured, populations. In a study in China males, unmarried persons, persons with a low education level and those with rural residence had worse responses to TKI-therapy and worse survival compared with controls [13]. At a recent global CML meeting in Bordeaux in September, 2019, researchers from several other countries including Argentina and Columbia reported worse survival in persons with CML * Robert Peter Gale [email protected]
Journal Title: Leukemia
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!