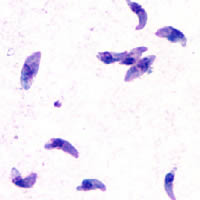
Photo from wikipedia
The opioid epidemic is a major societal problem that has led to reevaluation of opioids as the mainstream treatment for chronic pain. Reports estimate that millions of people misuse opioids… Click to show full abstract
The opioid epidemic is a major societal problem that has led to reevaluation of opioids as the mainstream treatment for chronic pain. Reports estimate that millions of people misuse opioids on an annual basis, particularly prescription opioid medications. Opioid administration, in individuals with and without pain, can result in an increased pain state, or hyperalgesia. Indeed, this effect can persist for some time following “recovery” from injury or surgery, termed “latent sensitization”. [1] Understanding the cellular and molecular basis of these opioid-dependent adaptations is important for utilizing opioids more effectively and identifying novel treatments. In this issue of Neuropsychopharmacology, the studies by Laboureyras et al. [2] focused on examining the effects of previous history of opioid exposure for acute pain and/or inflammation on subsequent response to opioid drugs. Rats were treated subcutaneously with high dose fentanyl, a common opioid used in the clinic for acute pain relief, alone or in combination with an injection of carrageenan, a compound that elicits a short-term inflammatory insult to approximate tissue injury in surgical clinics. The purpose of the studies was to determine if latent sensitization alters the effects of opioids after recovery from hyperalgesia induced by carrageenan. The results show a striking biphasic response to a second administration of fentanyl. Although there is an expected shift in the dose-response to the right for analgesic effects of fentanyl (i.e., tolerance) in pain and opioid-experienced rats compared to naïve control rats, the second fentanyl administration also elicited a clear hyperalgesic phase. At ultralow fentanyl doses (ng/kg range), solely hyperalgesia was observed. At higher doses, analgesia was the primary response in naïve rats. In contrast, in pain/fentanyl-experienced rats, fentanyl produced a biphasic analgesia/hyperalgesia with increasing doses. Further studies identified spinal N-methyl-D-aspartate (NMDA) receptorinducible nitric oxide synthase (NOS) cascade as critical for both acute tolerance and hyperalgesia. Intriguingly, a polyamine deficient diet (PDD) decreased the development of fentanyl tolerance and hyperalgesia, and suppressed overactivation of NOS signaling. The authors conclude that the results indicate that a patient’s history of pain, prior opioid exposure and even nutrition should be considered in developing individualized management of pain relief. In considering the model used for these studies, it is important to note that nociceptive thresholds were defined using a modified Randall-Selitto method where a constant mechanical pressure is applied to the hind paw until the rat vocalizes. The rationale for using vocalization rather than typical paw withdrawal threshold is that vocalization is an integrated response versus the reflex response used in other standard pain tests like thermal tail-flick and von Frey mechanical testing. This is an interesting difference that may allow clearer measurement of hyperalgesic effects of ultra-low dose fentanyl but does make it more difficult to compare the results to the more general findings in the field. A second consideration is the clinical relevance of using fentanyl compared to other opioids such as hydrocodone, oxycodone, and morphine that are commonly prescribed. It would be interesting to determine if these other clinically relevant opioids produce strong hyperalgesia with single high dose administration given signaling bias of different opioid ligands to different intracellular signaling pathways. Latent sensitization is observed with morphine administration suggesting that opioid efficacy is not an important determinant in initiating signaling involved in the hyperalgesia. However, fentanyl has unique pharmacological and pharmacokinetic properties largely stemming from its lipophilicity that may contribute to the observed effects at ultra-low doses. [3] It should also be noted that although carrageenan is a short inflammatory insult, latent sensitization is observed over longer time periods with Complete Freund’s adjuvant (CFA), a persistent inflammation model. [1] An interesting point considered in the discussion of Laboureyras et al. is that a primary function of endogenous opioids may be to facilitate pain and contribute to the development and/or maintenance of hyperalgesia. This is based on prior work from this laboratory examining the ability of non-nociceptive stress to exacerbate pain, and studies from other laboratories showing increased endogenous opioid release with stress. As stress also alters release of other neuropeptides, the interpretation that a primary action of endogenous opioids is to facilitate pain is premature. However, the discussion of how opioids might contribute to both hyperalgesia and analgesia highlights a major gap in the opioid field – full characterization of the endogenous opioid system, including when, where and how much is released under which physiological conditions. Many of the endogenous opioid peptides have similar signaling profiles, [4] so direct comparisons of opioid peptides to fentanyl in studies such as these could provide novel insight into signaling pathways involved in opioid-mediated hyperalgesia. The good news is that with the development of new biosensors and a renewed interest in endogenous opioids, future research will soon be able to answer these questions in more detail.
Journal Title: Neuropsychopharmacology
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!