Photo from wikipedia
Inflammatory bowel disease (IBD) are characterized by a chronic course requiring a lifelong treatment, and an overall 25% of cases are diagnosed in the childhood. Both the adaptive and the… Click to show full abstract
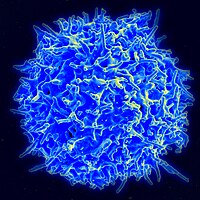
Inflammatory bowel disease (IBD) are characterized by a chronic course requiring a lifelong treatment, and an overall 25% of cases are diagnosed in the childhood. Both the adaptive and the innate immune systems are involved in the gut inflammation occurring in IBD. Several T helper cell subsets are known to promote inflammatory responses in the gut. Previous studies have reported that T helper(Th)−1 cells secrete key cytokines as interferon(IFN)-γ, tumor necrosis factor(TNF)-α, and interleukin(IL)−12 in Crohn disease (CD), and by contrast, Th2 cells with the production of IL-5, IL-9, and IL-13 are predominant in Ulcerative Colitis (UC). More recently, it was demonstrated that an additional helper T cell subset, Th17 cells, contributes to chronic intestinal inflammation including IBD. In adult IBD patients, mainly in UC individuals, Th17 cells and their related cytokines, as i.e., IL-17A and IL-22, were found increased in the serum and in the intestinal mucosa compared to control subjects. In addition, a positive correlation was found between the levels of Th17 cytokines or their mRNA expression and disease activity parameters, as endoscopic and histological grading, C-reactive protein and platelet levels. Though a great progress was reached in the comprehension of the immune mechanisms responsible of gut inflammation in adult subjects with IBD, very few studies focused on the immunological events involved in the development of IBD in pediatric age. Children affected by IBD seem to be a different population with distinctive immunological characteristics and often a more severe phenotype compared to IBD adults, and for this reason, further studies are necessary to better typify the early immune response that develops in pediatric IBD. Moreover, the research of biomarkers to distinguish between pediatric CD and UC could be important to facilitate IBD diagnosis and to establish new specialized approaches for the treatment. In this context, the study published by the Pediatric Research Journal from Busch and colleagues gives a relevant contribution to better understand the immunological features in the pathogenesis of pediatric IBD, and to propose a new potential diagnostic approach for this IBD cohort. They analyzed by quantitative polymerase chain reaction (qPCR) the expression of 16 target genes, that encode cytokines or transcription molecules in intestinal biopsies taken from fifty-two pediatric IBD and nonIBD individuals. In particular, they observed an overexpression of IL-17 mRNA in the tissues from IBD patients, mainly UC, compared to the control group, and also an increased expression of IL-22 in UC relative to CD intestinal samples. The elevated levels of both cytokines IL-17 and IL-22 produced by Th17 cells in intestinal mucosa highlight the contribution of this cell subset non only in adult but also in pediatric IBD mucosal lesions. Accordingly, previous studies found an increase of Th17 effector cells paralleled by a reduction of Treg cells in the peripheral blood of IBD children. More specifically, the involvement of Th17 cells found by the authors in particular in the tissue specimens of UC compared to CD patients, is probably due to the different molecular pathway at the base of the pathogenesis of the two IBD conditions. The identification of key cytokines unique for UC or CD, could enhance the current understanding of their pathogenesis. As well known, Th17 cells possess a great functional and phenotypical plasticity, and in response to environmental condition they can acquire the ability to produce Th1/Th2 cytokines in addition to IL-17. In particular, in inflammatory states, Th17 cells can change into a Th17/Th1 or Th17/Th2 phenotype, and the “shifted” cells seems to be more pathogenic and aggressive than the “unshifted” cells. The existence of T lymphocytes at the same time producing both IL-17 and IFN-γ identified as Th17/Th1, as well as both IL-17 and IL-4 identified as Th17/Th2, was shown in intestine inflammatory conditions. Th1 cells generated from Th17 cells were defined as non-classical Th1 to discern them from classical Th1, which instead are derived from the direct differentiation of naïve T cells. The transition of Th17 to nonclassic Th1 subset could be mediated by different factors including TNF-α, and the same Th17cells produce TNF-α and therefore with autocrine or paracrine mechanism can drive the shifting to Th1. Although it has been demonstrated an inflammatory function of Th17 cells and Th17-related cytokines in the disease activity and in the mucosal damage, Busch et al. proposed also a protective role of this T cell population in IBD. The authors hypothesize that the increased IL-17A gene expression found mainly in UC children, could represent a response to, rather than the cause of bowel inflammation. Most of the experimental data on the regulatory function of Th17 cells has been observed in murine colitis models. The transdifferentiation of Th17 cells into regulatory T cells, a process of global genetic reprogramming, was assessed by a Th17 cell-mediated colitis model in which Th17 cells completed their functional conversion contributing to the resolution of inflammation. However, in humans the antibodies against IL-17A protein or IL-17A receptor have been successfully used in some inflammatory pathologies, such as psoriasis and rheumatoid arthritis, but on the contrary with poor results in IBD.
Journal Title: Pediatric Research
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!