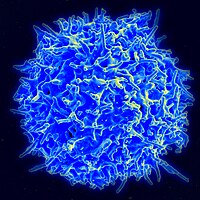
Photo from wikipedia
Effective immune control of the viral reservoir during antiretroviral therapy (ART) in human immunodeficiency virus (HIV)-infected patients is predominantly mediated by cellular immunity and CD8 T cells. In a recent… Click to show full abstract
Effective immune control of the viral reservoir during antiretroviral therapy (ART) in human immunodeficiency virus (HIV)-infected patients is predominantly mediated by cellular immunity and CD8 T cells. In a recent work, Jin et al. highlighted the direct role of unconventional CD45RAPanKIREOMESNKG2A memory T cells in the effective reduction in the latent viral reservoir during ART in HIV-infected patients. The authors nicely proposed a mechanism by which unconventional antigen-inexperienced memory CD8 T cells rather than antigen-specific CD8 T cells detect and kill reactivating HIV-infected cells through counter inhibition of HLA-I/KIR signaling. Since its first description in the 1980s, great progress has been made in developing a treatment for HIV infection. Despite high efficiency in suppressing viremia and preventing transmission, ART is not curative and has to be taken for life. Indeed, in the vast majority of cases, viral replication resumes if ART is discontinued due to the persistence of the viral reservoir. The retrovirus HIV-1 integrates its proviral genome into the host genome of infected target cells, such as activated CD4 T cells. Although most target CD4 T cells quickly die upon infection, a small proportion of these infected cells survive after having integrated the proviral DNA, which then persists indefinitely. Such a latent reservoir has a very slow decay, and as a consequence, treatment is unfortunately almost never curative. Evidence indicates that effector CD8 T cells, rather than antibodies, play a major role in the control of HIV-1 through the control of disease development and viral transmission. However, conventional viral-specific cytotoxic T cells (CTLs) might not be the only players in controlling the latent reservoir. Indeed, while conventional CTLs effectively limit viral burden in elite controllers, conventional HIV-specific CTL responses in ART patients cannot effectively eradicate latent reservoirs. Over the last decade, several studies in mice have comprehensively described the existence of an unconventional population of memory CD8 T cells that arise in response to environmental cues rather than antigen stimulation. This population of memory-phenotype CD8 T cells is antigen-inexperienced and is named innate or virtual memory CD8 T (CD8 TVM) cells. 7 CD8 TVM cells display most of the functions of “true” or antigen-experienced memory cells, including increased effector capacities against pathogens, independent of the encounter with a specific antigen. While CD8 TVM cell biology has been widely described in mice, studying antigeninexperienced populations in humans is complicated by the nearly impossible task of controlling previous exposure to foreign antigens such as pathogens. Nonetheless, there is evidence for the existence of “memory T cells with naive phenotype”, including CD45RA CD8 T cells displaying memory features. These cells have been described as CD45RA CD45ROCD27EOMEST-BET and/or NKG2AKIR2DKIR3DL1. Given the effector potential of CD8 TVM cells, the study by Jin et al. provides a thorough investigation of these unconventional memory-phenotype CD8 T cells and provides some important demonstrations that CD8 TVM cells have an important role in the control of HIV infection in ART patients. A population of expanded unconventional CD45RAPanKIR and/or NKG2A CD8 T cells was found to be present in HIV-infected individuals. These CD8 TVM cells displayed increased levels of NK receptors, CD122, EOMES, and T-BET, lower levels of PD-1 and increased effector features, both cytotoxic and noncytotoxic. Although it is very difficult to be conclusive about the true identity of these CD8 TVM cells, they nonetheless constitute a population of CD8 T lymphocytes with innate-like properties. This population was present in an increased number in HIV patients (treatment naive or receiving ART) compared to healthy controls and negatively correlated with HIV DNA and cell-associated unspliced RNA. Interestingly, the proportions of CD8 TVM cells among total CD8 T cells positively correlated with both serum IL-15 and IFN-α2 levels. While this finding might be anticipated from the characteristics of CD8 TVM cells in mice, it suggests a reason for why some people develop those cells more steadily and potentially control HIV infection better than other patients. For example, we and others have shown that a history of infection, notably by helminths, can influence the proportion of CD8 TVM cells in mice, 10 but it is still unclear whether a similar mechanism exists in humans. How this population of CD8 TVM cells develops in humans and therefore how it can be manipulated in the context of treatment or vaccination is of great interest. Another important question concerns the mechanisms by which CD8 TVM cells allow better control of viral infections. In this study, although showing responsiveness to HIV peptides, the CD8 TVM cell population from ART patients was not specifically enriched with HIV-specific CD8 TVM cells, consistent with innatelike and bystander functions of those cells. The capacity of CD8 TVM cells to control HIV appeared to be inhibited by HLA-I/KIR signaling. However, it remains unclear whether these cells develop bystander defenses independently of virus-specific recognition or whether the control of HIV virus is regulated by virus-specific CD8 TVM cells. Of course, both mechanisms could be present, and the population of CD8 TVM cells described here could even show a