Photo from wikipedia
1Institute of Neuroscience and Medicine: Brain and Behaviour (INM-7), Jülich Research Centre, Jülich, Germany. 2Institute of Systems Neuroscience, Medical Faculty, Heinrich Heine University Düsseldorf, Düsseldorf, Germany. ✉e-mail: [email protected] Due to… Click to show full abstract
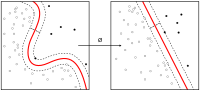
1Institute of Neuroscience and Medicine: Brain and Behaviour (INM-7), Jülich Research Centre, Jülich, Germany. 2Institute of Systems Neuroscience, Medical Faculty, Heinrich Heine University Düsseldorf, Düsseldorf, Germany. ✉e-mail: [email protected] Due to a lack of objective biomarkers, psychiatric diagnoses still rely strongly on patient reporting and clinician judgement. The ensuing subjectivity negatively affects the definition and reliability of psychiatric diagnoses1,2. Recent research has suggested that a combination of advanced neuroimaging and machine learning may provide a solution to this predicament by establishing such objective biomarkers for psychiatric conditions, improving the diagnostic accuracy, prognosis and development of novel treatments3. These promises led to widespread interest in machine learning applications for mental health4, including a recent paper that reports a biological marker for one of the most difficult yet momentous questions in psychiatry—the assessment of suicidal behaviour5. Just et al. compared a group of 17 participants with suicidal ideation with 17 healthy controls, reporting high discrimination accuracy using task-based functional magnetic resonance imaging signatures of lifeand death-related concepts3. The authors further reported high discrimination between nine ideators who had attempted suicide versus eight ideators who had not. While being a laudable effort into a difficult topic, this study unfortunately illustrates some common conceptual and technical issues in the field that limit translation into clinical practice and raise unrealistic hopes when the results are communicated to the general public. From a conceptual point of view, machine learning studies aimed at clinical applications need to carefully consider any decisions that might hamper the interpretation or generalizability of their results. Restrictiveness to an arbitrary setting may become detrimental for machine learning applications by providing overly optimistic results that are unlikely to generalize. As an example, Just et al. excluded more than half of the patients and healthy controls initially enrolled in the study from the main analysis due to missing desired functional magnetic resonance imaging effects (a rank accuracy of at least 0.6 based on all 30 concepts). This exclusion introduces a non-assessable bias to the interpretation of the results, in particular when considering that only six of the 30 concepts were selected for the final classification procedure. While Just et al. attempt to address this question by applying the trained classifier to the initially excluded 21 suicidal ideators, they explicitly omit the excluded 24 controls from this analysis, preventing any interpretation of the extent to which the classifier decision is dependent on this initial choice. From a technical point of view, machine learning-based predictions based on neuroimaging data in small samples are intrinsically highly variable, as stable accuracy estimates and high generalizability are only achieved with several hundreds of participants6,7. The study by Just et al. falls into this category of studies with a small sample size. To estimate the impact of uncertainty on the results by Just et al., we adapted a simulation approach with the code and data kindly provided by the authors, randomly permuting (800 times) the labels across the groups using their default settings and computing the accuracies. These results showed that the 95% confidence interval for classification accuracy obtained using this dataset is about 20%, leaving large uncertainty with respect to any potential findings. Special care is also required with respect to any subjective choices in feature and classifier settings or group selection. While ad-hoc selection of a specific setting is subjective, testing of different ones and outcome-based post-hoc justification of such leads to overfitting, thus limiting the generalizability of any classification. Such overfitting may occur when multiple models or parameter choices are tested with respect to their ability to predict the testing data and only those that perform best are reported. To illustrate this issue, we performed an additional analysis with the code and data kindly provided by Just et al. More specifically, in the code and the manuscript, we identified the following non-exhaustive number of prespecified settings: (1) removal of occipital cortex data; (2) subdivision of clusters larger than 11 mm; (3) selection of voxels with at least four contributing participants in each group; (4) selection of stable clusters containing at least five voxels; (5) selection of the 1,200 most stable features; and (6) manual copying and replacing of a cluster for one control participant. Importantly, according to the publication or code documentation, all of these parameters were chosen ad hoc and for none of these settings was a parameter search performed. We systematically evaluated the effect of each of these choices on the accuracy for differentiation between suicide ideators and controls in the original dataset provided by Just et al. As shown in Fig. 1, each of the six parameters represents an optimum choice for differentiation accuracy in this dataset, with any (even minor) change often resulting in substantially lower accuracy estimates. Similarly, data leakage may also contribute to optimistic results when information outside the training set is used to build a prediction model. More generally, whenever human interventions guide the development of machine learning models for the prediction of clinical conditions, a careful evaluation and reporting of any researcher’s degrees of freedom is essential to avoid data leakage and overfitting. Subsequent sharing of data processing and analysis pipelines, as well as collected data, is a further key step to increase reproducibility and facilitate replication of potential findings. For the field of clinical neuroscience to move towards being able to improve the diagnosis and prognosis of psychiatric conditions using objective machine learning-based biomarkers in mental health, it is crucial to deal with the above conceptual and technical pitfalls in the first place. Most importantly, realistic clinical populations need to be enrolled in such studies to increase the ecological validity and generalizability. Furthermore, strict technical and operational procedures need to be defined. At the stage Towards increasing the clinical applicability of machine learning biomarkers in psychiatry
Journal Title: Nature human behaviour
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!