Photo from wikipedia
Nature reviews | CliniCal OnCOlOgy The propensity to become cancerous is often apparent in the genome many years before transformation Clinical surveillance of individuals with Barrett’s oesophagus, whose risk of… Click to show full abstract
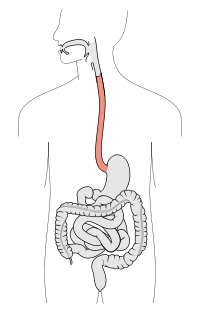
Nature reviews | CliniCal OnCOlOgy The propensity to become cancerous is often apparent in the genome many years before transformation Clinical surveillance of individuals with Barrett’s oesophagus, whose risk of progression to oesophageal adenocarcinoma is ~0.3% per year, involves histopathological examination of endoscopy-derived tissue. Genomic instability (including copy number alterations) has been proposed as a risk factor for Barrett’s oesophagus progression and is now the basis of a new prediction model that could facilitate earlier management of individuals at high risk of developing cancer. the discovery cohort of this study involved 45 individuals who had progression to adenocarcinoma after a minimum follow up of 1 year after diagnosis of nondysplastic Barrett’s oesophagus (‘progressors’) and 43 individuals without progression after a minimum follow-up duration of 3 years (‘non-progressors’). Both groups were demographically matched. Copy-number instability information from 777 endoscopy-derived samples from the discovery cohort was obtained through shallow whole-genome sequenc ing and used to generate a logis tic regression model of progression, which was subsequently validated in two independent cohorts (213 and 1,272 samples from 76 and 248 individuals, respectively). the model distinguished three groups according to the probability of progression to adenocarcinoma: low (probability ≤0.3), moderate and high (≥0.5). Non-dysplastic samples from the discovery and validation cohorts were classified with the model: 60.5% and 77% of samples, respectively, from progressors were classified as ‘high risk’, and 64.7% and 55% of non-dysplastic samples from non-progressors as ‘low risk’. among progressors, 50% had at least one sample classified as high risk ≥8 years before dysplastic transformation had been detected. “the propensity to become cancerous is often apparent in the genome many years before transformation,” explains co-lead investigator Moritz Gerstung. if the model had been available to classify the second endoscopy sample available for each individual in the discovery cohort and for subsequent clinical decision-making according to current treatment criteria, 54% of progressors would have received earlier treatment and 51% of non-progressors would have had less frequent endoscopies. “we plan to determine whether we can increase the precision of this model by adding factors such as smoking history or BMi,” comments co-lead investigator rebecca Fitzgerald, adding: “the model will be tested in a randomized trial before it can be proposed as part of routine clinical practice”.
Journal Title: Nature Reviews Clinical Oncology
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!