Photo from wikipedia
Viral infection is more frequently reported in cord blood transplantation (CBT) than in transplantation of other stem cell sources, but its precise mechanism related to antiviral host defenses has not… Click to show full abstract
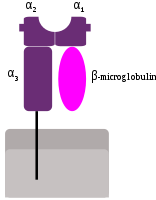
Viral infection is more frequently reported in cord blood transplantation (CBT) than in transplantation of other stem cell sources, but its precise mechanism related to antiviral host defenses has not been elucidated yet. To evaluate the effect of human leukocyte antigen (HLA) class I allele-level incompatibility on viral infection in CBT, we conducted a single-center retrospective study. Total 94 patients were included, and viral infections were detected in 32 patients (34%) within 100 days after CBT. HLA-C mismatches in graft-versus-host direction showed a significantly higher incidence of viral infection (hazard ratio (HR), 3.67; p = 0.01), while mismatches in HLA-A, -B, or -DRB1 were not significant. Overall HLA class I mismatch was also a significant risk factor and the predictor of post-CBT viral infection (≥ 3 mismatches, HR 2.38, p = 0.02), probably due to the insufficient cytotoxic T cell recognition and dendritic cell priming. Patients with viral infection had significantly worse overall survival (52.7% vs. 72.1%; p = 0.02), and higher non-relapse mortality (29.3% vs. 9.8%; p = 0.01) at 5 years. Our findings suggest that appropriate graft selection as well as prophylaxis and early intervention for viral infection in such high-risk patients with ≥ 3 HLA class I allele-level mismatches, including HLA-C, may improve CBT outcomes.
Journal Title: Scientific Reports
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!