Photo from wikipedia
Abstract Introduction: Brain parenchymal abscesses are relatively infrequent but potentially serious infections in the paediatric population. Surgical intervention in addition to a prolonged administration of antibiotics is generally appropriate management.… Click to show full abstract
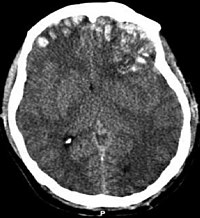
Abstract Introduction: Brain parenchymal abscesses are relatively infrequent but potentially serious infections in the paediatric population. Surgical intervention in addition to a prolonged administration of antibiotics is generally appropriate management. This study presents our centre’s experience of managing such patients in the context of relevant literature. Method: A single-centre retrospective case note review was conducted over a 15 year period (2003–2017). Patients were selected from electronic hospital records using ICD10 code G06.0. Patients < 18 years of age with a confirmed intra-parenchymal abscess were included. Patient records were reviewed for abscess location, microbiology results, surgical intervention, and outcome using the Glasgow Outcome Score at 3 months. Results: Twenty-four patients were identified (mean age: 7.4 ± 5.3 years, male n = 11). Twelve (50.0%) patients had an abscess in the frontal lobe and Streptococcus was the most common causative microorganism (n = 15). Nineteen patients (79.2%) had an identifiable source which included: ENT infections, congenital cardiac malformations, recent dental surgery and meningitis. All 24 patients underwent surgery with 20 patients having a total of 32 aspirations between them and the other 4 having craniotomy and excision. Twenty patients had 3 month follow-up data of which 18 patients scored GOS: 5, one was GOS: 4 and one was GOS: 3. Conclusions: Brain parenchymal abscess remains an uncommon pathology in the paediatric population. The majority of patients have a preceding infection with Streptococcus as the most common causative organism. Antimicrobial therapy should be selected accordingly. All of our patients underwent surgical intervention and received intravenous antibiotics with favourable outcome and no mortality.
Journal Title: British Journal of Neurosurgery
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!