Photo from wikipedia
Abstract Objectives To evaluate the trend in cytogenetic/molecular testing rate in chronic lymphocytic leukemia (CLL) and assess the clinical and economic burden of first-line (1 L) treatment with chemoimmunotherapy (CIT) by… Click to show full abstract
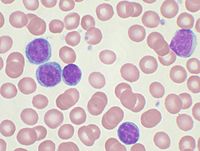
Abstract Objectives To evaluate the trend in cytogenetic/molecular testing rate in chronic lymphocytic leukemia (CLL) and assess the clinical and economic burden of first-line (1 L) treatment with chemoimmunotherapy (CIT) by risk status. Methods This retrospective cohort study identified patients with CLL from a U.S. managed care population. Medical records were obtained for eligible patients who initiated 1 L CIT between 1/1/2007 and 7/31/2019 and underwent prognostic testing to classify them as high risk (del(17p), TP53 mutation, del(11q), unmutated IGHV or complex karyotype) or as non-high risk by FISH only (non-del(17p) and non-del(11q)). Study outcomes included testing rate, time to next treatment (TTNT) or death, time to treatment failure (defined as time to change of therapy, non-chemotherapy intervention, hospice care or death), and total plan paid costs (medical + pharmacy) per patient per month (PPPM) in the 1 L period. Cox proportional hazard models and generalized linear models were used to calculate adjusted hazard ratio or rate ratio. Results Among the 1,808 patients with CLL, 612 were FISH or IGHV tested and the rate of testing increased from 30% to 44% from 2007–2019. High-risk patients (n = 119) had 65% higher risk of next treatment or death (median time: 2.4 vs 3.7 years), 65% higher risk of treatment failure (median time: 3.0 vs 4.9 years), and 33% higher costs ($12,194 vs $9,055, p = 0.027) during 1 L treatment than non-high risk patients (n = 134). Conclusions High-risk CLL patients treated with 1 L chemoimmunotherapy have poorer clinical and economic outcomes compared to non-high risk patients. Assessment of genetic risk remains suboptimal.
Journal Title: Current Medical Research and Opinion
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!