Photo from wikipedia
Bisphosphonate (BP) therapy is widely used for the treatment of both malignant and non-malignant bone diseases, frequently osteoporosis, Paget’s disease of bone, osteogenesis imperfecta, bone metastasis, and multiple myeloma, among… Click to show full abstract
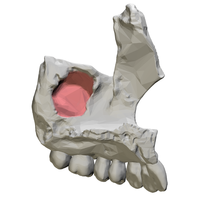
Bisphosphonate (BP) therapy is widely used for the treatment of both malignant and non-malignant bone diseases, frequently osteoporosis, Paget’s disease of bone, osteogenesis imperfecta, bone metastasis, and multiple myeloma, among others (1, 2). Despite its clinical benefits, treatment with BP is associated with a risk of developing a serious adverse effect: bisphosphonaterelated osteonecrosis of the jaws (BRONJ). As defined by the American Association of Oral and Maxillofacial Surgeons (3), a diagnosis of BRONJ must meet the following requirements: (i) exposed bone in the maxillofacial region over a period of 8 weeks; (ii) current or previous treatment with BP; and (iii) no prior history of radiation therapy to the jaws. According to the literature, BRONJ is prevalent only in the jaws and not in other areas of the body owing to the presence of two main conditions: the infected oral environment and the repetitive trauma inflicted on the jaws. Nevertheless, its exact initiating aetiology is still unclear (4, 5). Thus far, the scientific community has always highlighted the need for a precipitating factor or trigger event (6, 7) that initiates the development of the disease, such as tooth extractions, implant placements, torus, pressure sores, root canal therapy, poor oral hygiene, or involuntary trauma. However, some spontaneous BRONJ cases have started to be described in the literature. We present a rare case of spontaneous bisphosphonate-related osteonecrosis of the palate (BRONP) with secondary oral–nasal fistula. A 56-year-old woman visited her dentist with the complaint of an air leak through her mouth to her nose. Examination revealed a painless ulcer in the central–posterior part of the left hard palate, 5 mm in diameter, with a communication to her nasal cavity. There was no sign of soft-tissue infection around the oral–nasal fistula and there was no evidence of an underlying palatal torus or other lesions (Figure 1A). There were no traumatic or other inciting acute events that could be related to this finding. Nevertheless, her medical history was significant for osteoporosis secondary to a hysterectomy that had been treated with oral alendronate sodium for 7 years. She did not report any toxic habits such as tobacco or cocaine use. Her dentist performed a biopsy to rule out inflammatory vessel diseases. The histopathological examination revealed an inflammation and granulation tissue reaction. Blood tests ruled out immunocompromised situations such as AIDS and lymphoproliferative syndrome, and a smear did not detect any bacterial, viral, or fungal infections. Although the patient had no history of any recent dentoalveolar procedure or an underlying palatal torus, she nevertheless presented with exposure and necrosis of the palatal bone for more than 8 weeks. The lesion was diagnosed as spontaneous BRONP with secondary oral– nasal fistula. The alendronate sodium was stopped to avoid progression of the disease, the patient was treated with antiseptic irrigation (chlorhexidine digluconate 0.12%), and she was referred to us for surgical closure. Computed tomography (CT) imaging was obtained in an attempt to define the extent of the process. It revealed a limited extension of the bony necrosis to the fistula area, and a low-density nasal floor bone (Figure 1B). The patient underwent surgery under general anaesthesia. First, a mucoperiosteal flap around the fistula was performed to repair the nasal layer without tension. Then, a partial-thickness palatal flap was transferred to the defect and fixed to the mucosal edge with 4-0 polyglycolic sutures (Figure 1C). Her postoperative course was uneventful. She has been followed for more than 3 years and has no evidence of further osteonecrosis (Figure 1D). After obtaining her rheumatologist’s approval, the BP treatment was not taken again to avoid further episodes of BRONP. The study was approved by the Ethics Committee at Teknon Medical Center under number BPF, and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The patient accepted an informed consent agreement. After a comprehensive electronic database search in PubMed and Embase, we can conclude that this is the first reported case of spontaneous oral–nasal fistula related to BRONP. Scand J Rheumatol 2019;48:85–86 85
Journal Title: Scandinavian Journal of Rheumatology
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!