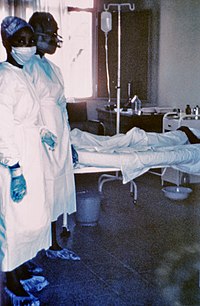
Photo from wikipedia
Platelets are increasingly recognized for their broad repertoire of activities spanning hemostatic, inflammatory, and immune continuums. In many cases, platelet functions cooperate to bridge these continuums, effectively triggering responses that… Click to show full abstract
Platelets are increasingly recognized for their broad repertoire of activities spanning hemostatic, inflammatory, and immune continuums. In many cases, platelet functions cooperate to bridge these continuums, effectively triggering responses that may act collectively and catalytically to mediate thrombotic, inflammatory, and immune activities [1–3]. These cooperative responses have led to the creation of the term “immunothrombosis,” which emphasizes the closely woven interplay between inflammation, immunity, and thrombosis. As the second most common circulating blood cell, platelets are centrally positioned in the vasculature to trigger immunothrombosis. Platelets possess a repertoire of intracellular and stored molecules (often in granule compartments that can be secreted) and surface anchored receptors. The array of proteins, lipids, and RNAs possessed by platelets allow these small anucleate cells to sense and respond to diverse signals, including those generated during infectious settings. For example, platelets possess the RNA and/or protein for nearly all toll-like receptors (TLRs) [4,5]. TLRs are one of the several surface ligands allowing viruses to bind to platelets. In addition to TLRs, platelets also express other binding proteins, including β3 integrin, DC-SIGN, and FcRyIIA, which enable virions to bind to, engage with, and/or enter platelets. In addition to these receptor-mediated interactions, platelets may also actively take up virions through a variety of other mechanisms, including clathrin-mediated endocytosis (CME) and pinocytosis [6]. Often, more than one factor is required for internalization of viruses by platelets. Systemic agonists and pathogen particles generated as viruses enter their host and replicate may also be sensed or recognized by platelets, leading to downstream activation responses and signaldependent binding to, and communication with, leukocytes. These molecules include danger-associated molecular patterns (DAMPs; including HMGB1, S100 proteins, interleukin 1 [IL-1] family members, type interferons [IFN], and tumor necrosis factor alpha [TNF-α]) and pathogen associated molecular patterns (PAMPs; including nucleic acid motifs, ssRNA, dsRNA, and unmethylated CpG motifs). Platelets, once activated, are primed to interact and aggregate with leukocytes (e.g., heterotypic aggregation). Increased platelet–leukocyte interactions can be observed in patients infected with influenza, SARS-CoV-2, and dengue infection – among others [7–12]. These interactions can promote inflammatory cytokine synthesis (such as MCP-1, IL-1β, IL-8, and IL-10), neutrophil extracellular trap (NET) formation, and antigen-dependent T cell responses [3,13,14]. Platelets also secrete numerous molecules, such as platelet factor 4 (PF4), RANTES, and P-selectin, which may directly or indirectly mediate the pathogenesis of viral infections. The net effect of these interactions is generally thought to promote immunothrombosis, although the full range of these interactions remains an active area of investigation. This mini-review series focuses on one class of pathogens, viruses, and their interactions with platelets. Over the last two years, interactions between platelets and viruses (particularly SARS-CoV-2) and the consequences of these interactions on the host have helped broaden our understanding of how virus directly and indirectly engage (and at times, enter) platelets and how this impacts subsequent physiological responses and clinical outcomes. Recent work on SARS-CoV-2 builds upon, and extends, earlier foundational work elucidating the role of platelets during other viral infections, including influenza, dengue, and hepatitis. While still incompletely understood, platelet responses to these viruses and generated signals may be physiologic or pathophysiologic. One example of a common, systemic, inflammatory agonist generated by the host during viral infections is interferon (IFN). Recent work has shown that the generation of IFN during viral infections induces the transcription and translation of IFNsensitive genes in megakaryocytes and platelets to augment host antiviral immune functions by megakaryocytes [15]. In other settings, viral infections promote injurious, platelet-driven cellular, soluble, and/or tissue responses. During SARS-CoV-2 infections, platelet activation is thought to contribute to the hypercoagulable state and a high incidence of thromboembolic complications in COVID-19 patients [16,17]. Similar platelet activation responses have been reported in other acute and chronic viral infections, including influenza and HIV. In addition to these functional activation responses, viruses (or agonists generated during viral infection) may also alter platelet number, typically leading to thrombocytopenia. The magnitude of the thrombocytopenia varies depending on the virus and clinical scenario, but in settings of severe dengue, the thrombocytopenia may be severe and associated with life-threatening bleeding. Despite the substantial progress made in this field, many important questions remain unanswered. For example, whether platelets express ACE2, the putative receptor for SARS-CoV-2, is controversial with some groups reporting the absence of ACE2 on human platelets and others finding the presence of ACE2 on platelets [7,18–20]. Additionally, although dengue virus replication within platelets has been convincingly demonstrated, whether or not that viral replication is productive is uncertain. Similar Correspondence: Matthew T. Rondina, Eccles Institute of Human Genetics, Room 4220 50 North Medical Drive, Salt Lake City, UT. Email: [email protected] http://www.tandfonline.com/iplt ISSN: 0953-7104 (print), 1369-1635 (electronic)
Journal Title: Platelets
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!