Photo from wikipedia
Abstract Iron deficiency anemia (IDA) affects more than 1.2 billion individuals globally. In addition to anemia, reactive thrombocytosis is also a common clinical hematological condition in patients with IDA. However,… Click to show full abstract
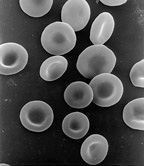
Abstract Iron deficiency anemia (IDA) affects more than 1.2 billion individuals globally. In addition to anemia, reactive thrombocytosis is also a common clinical hematological condition in patients with IDA. However, some case reports have described the thrombotic complications in association with IDA-induced thrombocytosis. Patients with a high risk of thrombosis need prompt identification and effective treatment to prevent thrombotic complications. While iron replacement treatment has been shown to decrease platelet count in this context, there is limited published evidence on how iron supplementation affects the thrombocytosis caused by IDA. We retrospectively examined the clinical records of 440 patients with IDA from an RCT completed from 1 January 2016, to 30 December 2017, and data obtained from this study was used for post hoc analysis to examine the effect of iron on platelet count in IDA-induced thrombocytosis. The mean ± standard deviation (SD) platelet counts of the 440 patients with IDA was 310.23 ± 98.72 × 109/L. With baseline platelet counts>450 × 109 /L as the cutoff for thrombocytosis, patients were divided into 2 groups: 36 (8.1%) in the IDA with thrombocytosis group (mean ± SD platelet count, 521.67 ± 73.85 × 109/L) and the remaining 404 in the IDA without thrombocytosis group (mean ± SD platelet count, 291.39 ± 76.11 × 109/L). Differences were found in baseline characteristics including white blood cell (WBC) count, hemoglobin (Hb) level, mean corpuscular volume (MCV), transferrin saturation (TSAT), serum iron (SI) level, and total iron-binding capacity (TIBC) between the two groups (P < .05). From baseline to 8 weeks of continuous iron supplementation treatment, the mean platelet counts in both groups were decreased at 2-week treatment intervals. And in the IDA with thrombocytosis group, half of the patients resolved thrombocytosis after 2 weeks of iron supplementation, and the counts of all patients with thrombocytosis decreased below 450 × 109 /L within 6 weeks. In conclusion, the rate of reactive thrombocytosis in patients with IDA was 8.1%. IDA patients with thrombocytosis showed more severe anemia, lower ferritin, and more advanced iron deficiency than those without thrombocytosis. Platelet counts of half of the patients with thrombocytosis reduced below cut off of 450 × 109/L for thrombocytosis after 2 weeks of treatment, and all patients resolved thrombocytosis after 6 weeks. Our study provided clinical evidence for more effective and individualized iron management in the future. IDA patients with thrombocytosis should take active iron treatment and increase follow-up frequency to prevent thrombotic events. For patients with persistent thrombocytosis, a concomitant clonal process should be considered.
Journal Title: Platelets
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!