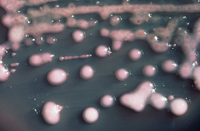
Photo from wikipedia
The spread of production of Klebsiella pneumoniae carbapenemase (KPC) b-lactamase enzyme among the Enterobacterales (EB), in particularly in Klebsiella pneumoniae (KPC-Kp), has become a worldwide health concern given the rising… Click to show full abstract
The spread of production of Klebsiella pneumoniae carbapenemase (KPC) b-lactamase enzyme among the Enterobacterales (EB), in particularly in Klebsiella pneumoniae (KPC-Kp), has become a worldwide health concern given the rising clinical burden of the associated infections. Despite the introduction of ceftazidime-avibactam (CZA) improved clinical outcomes, several reports attested the onset of CZA resistance among KPC-Kp. CZA resistance is mainly conferred by blaKPC mutations and was reported to occur more commonly following CZA treatment among patients with KPC-3-producing EB infection, pneumonia, and on renal replacement therapy. The recently approved meropenem-vaborbactam (MEV) showed high potency against KPC-producing EB given vaborbactam activity of both inhibition of class A carbapenemases and reduction of meropenem MICs to wild-type MIC levels and was successfully used as salvage therapy for CZA resistant KPC-Kp infection. Similarly, despite limited evidence on its clinical use is available so far, the old fosfomycin (FF) is currently considered a reliable option in combination therapy against KPC-Kp. This study aimed at investigating the efficacy of MEV in combination with FF to lay the in vitro foundations for assessing the potential contribution to both KPC-Kp infections management and prevent the development of resistance to novel drugs. Synergistic activity of MEV with FF was evaluated against 22 non-duplicate clinical isolates of KPC-Kp (Table 1) collected at the University Hospital Citt a della Salute e della Scienza in Turin, Italy. Antimicrobial susceptibility and synergy testing were carried out by the gradient diffusion method using MIC Test Strip (Liofilchem, Roseto degli Abruzzi, Italy), and the minimum inhibitory concentrations (MICs) were interpreted according to European Committee on Antimicrobial Susceptibility Testing (EUCAST) clinical breakpoints. The blaKPC genes of the KPC-Kp isolates were previously characterized by PCR and DNA sequencing. The 22 KPC-Kp isolates harboured blaKPC-2 (n1⁄4 7), blaKPC-3 (n1⁄4 7), blaKPC-31 (n1⁄4 5), blaKPC-33 (n1⁄4 2) and blaKPC-14 (n1⁄4 1). Among the isolates, 11 (50%) showed resistance to CZA, eight were resistant to FF, whereas four isolates (18.2%) were resistant to MEV, of which one was resistant to both CZA and MEV and FF. No in vitro synergistic activity was observed, whereas addictive and indifferent effects were shown in 77.3% (n1⁄4 17) and 22.7% (n1⁄4 5) of the isolates, respectively. KPC-Kp isolates that showed indifference to MEV and FF combination were all resistant to CZA. Of these, three showed resistance also to FF, one was also resistant to MEV and FF, Correspondence to: Matteo Boattini, Microbiology and Virology Unit, University Hospital Citt a della Salute e della Scienza di Torino, Corso Bramante 88/90, 10126, Turin, Italy. Email: [email protected] These authors contributed equally to this work. This article has been republished with minor changes. These changes do not impact the academic content of the article.
Journal Title: Journal of Chemotherapy
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!