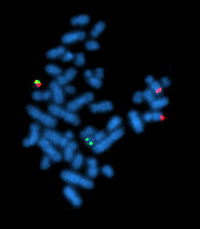
Photo from wikipedia
The management of patients with chronic myeloid leukemia (CML) has changed dramatically with the introduction of imatinib. Although many patients with CML in chronic phase (CML-CP) achieve and maintain durable… Click to show full abstract
The management of patients with chronic myeloid leukemia (CML) has changed dramatically with the introduction of imatinib. Although many patients with CML in chronic phase (CML-CP) achieve and maintain durable responses under imatinib, some need to be switched to alternative tyrosine kinase inhibitors (TKIs) due to intolerance and/or failure. After being first tested successfully in imatinib-resistant/-intolerant patients, second-generation TKIs (2GTKIs) (nilotinib, dasatinib, and bosutinib) were then utilized in the upfront setting and they were compared with imatinib among patients with CMLCP in three phase III prospective, randomized, companysponsored trials [1–3]. Although bosutinib was proven to be efficient among imatinib-resistant or -intolerant cases, it failed to demonstrate superior outcomes over imatinib in the BELA (Bosutinib Efficacy and Safety in Newly Diagnosed CML) trial, in which the primary end point was complete cytogenetic response (CCyR) at 12 months [3]. Although the rate of major molecular response (MMR) in the bosutinib arm was significantly superior than that of patients receiving imatinib (41% vs. 27%, p < 0.001) as a secondary end point, the primary end point was not different for bosutinib (70%) versus imatinib (68%) (p = 0.601); consequently, bosutinib was not approved as a frontline treatment option for patients with CML-CP since the primary end point was not met [3]. Also in that study it was shown that the rate of discontinuation due to adverse events (AEs) was higher in patients receiving bosutinib 500 mg/day (19% – 48 patients) when compared to imatinib 400 mg daily (6% – 14 patients), and 15 (31%) of these 48 patients discontinued bosutinib before initial assessment, which might be one of the reasons for the low CCyR rates in the bosutinib arm. Gastrointestinal AEs were more common with bosutinib, such as diarrhea (70% vs. 26 %; p < 0.001), vomiting (33% vs. 16 %; p < 0.001), and alanine aminotransferase elevation (33% vs. 9 %; p < 0.001) [4]. In contrast, the hematologic and non-hematologic AEs that were less common with bosutinib were edema (peripheral, 5% vs. 12%; p = 0.006; periorbital, 2% vs. 14%; p < 0.001), musculoskeletal complaints (muscle cramps, 5% vs. 22%; p < 0.001; myalgia, 5% vs. 12%; p = 0.010; bone pain, 4% vs. 11%; p = 0.003), and neutropenia (13% vs. 30%; p < 0.001) [4]. The initial results of another multicenter phase III trial comparing frontline bosutinib 400 mg/day with imatinib 400 mg daily (ClinicalTrials.gov identifier: NCT02130557) were recently presented at an international meeting [5]. Receiving a lower daily dose of bosutinib than that of BELA trial, patients on bosutinib had significantly higher rates of MMR and CCyR at 12 months and achieved responses faster than those on imatinib. In the near future, the results of this trial would most probably make bosutinib to be the fourth treatment option for newly diagnosed patients with CML-CP. However as in the BELA trial, more patients receiving bosutinib needed to stop TKI therapy because of toxicity than that of imatinib arm, and the percentage of patients who needed to discontinue the study drug due to drug-induced AEs in bosutinib and imatinib arms were 12.7% and 8.7%, respectively [5]. In addition to these treatment options, ponatinib is a panBCR/ABL1 inhibitor, which potently inhibits all ABL mutations including T315I. After the successful results in the salvage setting, ponatinib was tested as a frontline agent in newly diagnosed CML-CP patients [6]. In EPIC (Ponatinib in Newly Diagnosed Chronic Myeloid Leukemia) trial, patients were randomized to receive ponatinib 45 mg daily or imatinib 400 mg daily; however, the study was terminated after a median follow-up of 5 months due to mainly arterial thrombotic events [6]. Knowing the fact that 2GTKIs are more potent than imatinib with lower rates of transformation to advanced disease (AD), these drugs are thought to be a better treatment option over imatinib in the upfront setting. Nilotinib and dasatinib were shown to be superior to imatinib regarding the speed and the depth of responses, but up to date, these drugs did not demonstrate a significant benefit in the long-term outcomes including progression-free and overall survivals (PFS and OS) over imatinib, when used as a frontline treatment option in patients with CMLCP. Although the rates may differ between different TKIs, all TKIs have hematologic AEs mainly appearing in the initial period of the tyrosine kinase inhibition. Some of the non-hematologic AEs are more related to a particular drug (e.g. dasatinib→pleural
Journal Title: Expert Review of Hematology
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!