Photo from wikipedia
PURPOSE To aim of this study is to investigate the prognostic value of using the NINDS standardized imaging-based pathoanatomic descriptors for the evaluation and reporting of acute TBI lesions. METHODS… Click to show full abstract
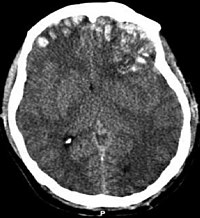
PURPOSE To aim of this study is to investigate the prognostic value of using the NINDS standardized imaging-based pathoanatomic descriptors for the evaluation and reporting of acute TBI lesions. METHODS For a total of 3,392 patients (2,244 males and 1,148 females, Median = 51 years) enrolled in the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study, we extracted 96 CDEs from the structured reports, spanning all three levels of pathoanatomic information (i.e. 20 "basic", 60 "descriptive" and 16 "advanced" CDE variables per patient). 6-month clinical outcome scores were dichotomized into favorable (GOS-E = 5-8) versus unfavorable (GOS-E = 1-4). Regularized logistic regression models were constructed and compared using the optimism-corrected AUC. RESULTS An abnormality was reported for the majority of patients (64.51%). In 79.11% of those patients, there was at least one coexisting pathoanatomic lesion or associated finding. An increase in lesion severity, laterality and volume was associated with more unfavorable outcomes. Compared to the full set of pathoanatomic descriptors (i.e. all three categories of information), reporting "basic" CDE information provides at least equal discrimination between patients with favorable versus unfavorable outcome (AUC = 0.8121 vs. 0.8155, respectively). Addition of a selected subset of "descriptive" detail (i.e. location and volume) to specific basic CDEs could improve outcome prediction (AUC = 0.8248). Addition of "advanced" or "emerging" information had minimal prognostic value. CONCLUSION Our results show that the NINDS standardized-imaging based pathoanatomic descriptors can be used in large-scale studies and provide important insights into acute TBI lesion patterns. When used in clinical predictive models, they can provide excellent discrimination between patients with favorable and unfavorable 6-month outcomes. If further validated, our findings could support the development of structured and itemized templates in routine clinical radiology. Key words: Traumatic Brain Injury, Computed Tomography, Common Data Elements, Structured Reporting.
Journal Title: Journal of neurotrauma
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!