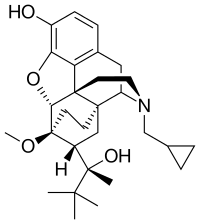
Photo from wikipedia
Opioid use disorder (OUD) is a national crisis. Health care must achieve greater success than it has to date in helping opioid users achieve recovery. Integration of comprehensive primary care… Click to show full abstract
Opioid use disorder (OUD) is a national crisis. Health care must achieve greater success than it has to date in helping opioid users achieve recovery. Integration of comprehensive primary care with treatment for OUD has the potential to increase care access among the substance-using population, improve outcomes, and reduce costs. However, little is known about the effectiveness of such care models. The Comprehensive Care Practice (CCP), a primary care practice located in Maryland, implemented a care model that blends buprenorphine treatment for OUD with attention to primary care needs. This study evaluates the model by comparing patients with OUD treated in CCP and other Maryland facilities in a large state Medicaid program. Compared to the non-CCP patient group (n = 867), the CCP group (n = 131) had a higher 6-month buprenorphine treatment retention rate (79% vs. 61%, adjusted average marginal effect (AME) = 0.17, P < 0.001). CCP patients also had fewer hospital stays in the 12-month follow-up period (0.22 vs. 0.41, AME = -0.17, P = 0.005), and lower total cost (US$10,942 vs. $13,097, AME = -$4554, P < 0.001) and hospital stay cost (US$1448 vs. $4265, AME = -$2609, P = 0.001), but higher buprenorphine pharmacy cost (US$3867 vs. $2781, AME = $987, P < 0.001). Other measures, including emergency department utilization and cost, substance abuse cost, and non-buprenorphine pharmacy cost, were not statistically different between the 2 groups. Results suggested that patients, as well as the health care system, can benefit from an integrated model of buprenorphine treatment and primary care for OUD with better treatment retention, fewer hospital stays, and lower costs.
Journal Title: Population health management
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!