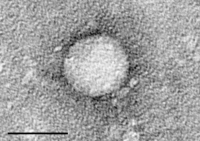
Photo from wikipedia
Chemotherapy-induced immunosuppression can lead to hepatitis B virus (HBV) reactivation in cancer patients. Both HBV carriers and individuals with serological signs of previously resolved HBV exposure are under the risk… Click to show full abstract
Chemotherapy-induced immunosuppression can lead to hepatitis B virus (HBV) reactivation in cancer patients. Both HBV carriers and individuals with serological signs of previously resolved HBV exposure are under the risk of severe hepatitis and liver failure during and after chemotherapy. The objective of this largest retrospective study was to analyze the consequences of HBV status in children receiving chemotherapy. A total of 479 patients (273 boys and 206 girls) aged 1-211 months diagnosed with acute hematologic malignancies and solid tumors were included in the study. Serological markers for HBV before and after chemotherapy and clinical data of the patients were evaluated retrospectively. Two hundred thirty-four of the participants were found to have protective antibody titers to HBV at admission. Five children were carrying HBV before chemotherapy. They received antiviral therapy during treatment and no reactivation was detected. Antibody against hepatitis B surface antigen (antiHBs) remained positive in 194 patients after chemotherapy. However, 17.09% (40/234) lost antiHBs positivity. In this group, three patients (1.28%) who initially had positive antiHBs and antihepatitis B core antibody experienced HBV reactivation and lost their protective antiHBs at the end of the therapy. Median antiHBs titer significantly decreased after chemotherapy (213.14 [range: 24-888] vs. 180.85 [range: 0-850]) (p = 0.0094). The current relatively large trial demonstrated that protective antibody titers remarkably altered after chemotherapy, and at least 17% of the pediatric oncology cases lost antiHBs positivity. Therefore, vaccine prevention and close monitoring of serology should be considered during chemotherapy.
Journal Title: Viral immunology
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!