Photo from wikipedia
Type 2 myocardial infarction (MI) is characterised by a functional imbalance between myocardial oxygen supply and demand in the absence of a thrombotic process, leading to myocardial necrosis. This type… Click to show full abstract
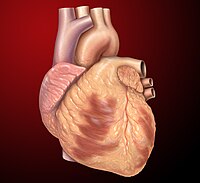
Type 2 myocardial infarction (MI) is characterised by a functional imbalance between myocardial oxygen supply and demand in the absence of a thrombotic process, leading to myocardial necrosis. This type of MI was relatively unknown among clinicians until the third universal definition of MI was published in 2017, differentiating Type 2 from Type 1 MI, which follows an acute atherothrombotic event. The pathogenesis, diagnostic and therapeutic aspects of Type 2 MI are described in the present review. Type 2 MI is a condition that is strongly linked to age because of vascular ageing concerning both epicardic vessels and microcirculation, age-related atherosclerosis and stress maladaptation. This condition predominantly affects multimorbid individuals with a history of cardiovascular disease. However, the conditions that lead to the functional imbalance between oxygen supply and demand are frequently extra-cardiac (e.g. pneumonia or anaemia). The great heterogeneity of the underlying etiological factors requires a comprehensive approach that is tailored to each case. In the absence of evidence for the benefit of invasive reperfusion strategies, the treatment of Type 2 MI remains to date essentially based on the restoration of the balance between oxygen supply and demand. For older co-morbid patients with Type 2 MI, geriatricians and cardiologists need to work together to optimise etiological investigations, treatment and prevention of predisposing conditions and precipitating factors.
Journal Title: Age and ageing
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!