Photo from wikipedia
Esophageal cancer invading the descending aorta is a frequent subset of locally advanced unresectable esophageal cancer. Radical resection combined with removal of the descending aorta may be the only possible… Click to show full abstract
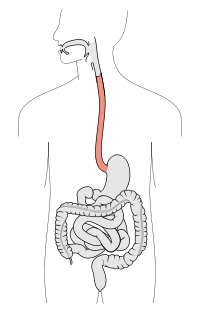
Esophageal cancer invading the descending aorta is a frequent subset of locally advanced unresectable esophageal cancer. Radical resection combined with removal of the descending aorta may be the only possible surgical approach for such tumors. [Case report] A 58-year-old man who complained of dysphagia was referred to our hospital. Esophagogastroscopy showed the presence of long-segment Barrett's esophagus 19 cm from the incisors and a type 2 tumor 29–38cm from the incisors. Computed tomography revealed that the metastatic lymph node had markedly invaded the descending aorta and showed left adrenal gland metastasis. This patient was diagnosed with Stage IV lower thoracic Barrett's esophageal adenocarcinoma. The patient was treated with two courses of cisplatin plus 5-fluorouracil. After the chemotherapy, the main tumor, left adrenal gland metastasis and lymph node metastasis had not responded. We judged that R0 surgery was available for excision of the aorta because the distant metastasis was only left adrenal metastasis and there was no emergence of a new lesion. [Surgery] First we operated the neck and abdomen simultaneously in the supine position. Superior mediastinal dissection and esophageal transection were performed by mediastinoscope-assisted transhiatal esophagectomy technique. Removal of the left adrenal gland and abdominal esophageal transection were performed. The position of the patient was converted to the left lateral position. With left thoracotomy, the descending aorta was taped above and below the lesion. With ACT 200 or more by heparin administration, PCPC was provided. Transfer descending aorta was replaced with artificial blood vessel. After neutralization by protamine sulfate, the thoracic esophagus was safely removed. The artificial blood vessel was covered with omentum and indwelling thoracic drain was performed. Finally, an esophagocutaneous fistula was built in the anterior chest. The operation time was 14h38min, and the blood loss was 1730g with 2970ml blood transfusion. The patient stayed in the ICU for seven days and discharge was 22 days post-operative. Histopathological diagnosis is adenocarcinoma of Barrett's esophagus, 80 × 30mm, por>tub2, pT4b (aorta). Bilateral thoracotomy is necessary in radical surgery for aortic infiltrating thoracic esophageal cancer, but surgical stress is excessive. A mediastinoscope-assisted transhiatal esophagectomy approach is a minimally invasive option to avoid bilateral thoracotomy. All authors have declared no conflicts of interest.
Journal Title: Diseases of the Esophagus
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!