Photo from wikipedia
Left ventricular assist device (LVAD) surgery improves quality of life (QoL) in chronic heart failure patients. Hemodynamic optimization of the LVAD therapy can improve patient outcomes, and potentially further improve… Click to show full abstract
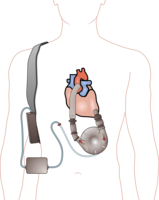
Left ventricular assist device (LVAD) surgery improves quality of life (QoL) in chronic heart failure patients. Hemodynamic optimization of the LVAD therapy can improve patient outcomes, and potentially further improve QoL in these patients. In this analysis, we assessed the improvement of the QoL post-LVAD surgery in patients with hemodynamic guided management by the CardioMEMS. Ten patients suffering from chronic heart failure, who underwent (semi-)elective LVAD surgery and participated in the HEMO-VAD pilot study, were included in this analysis. All patients received a CardioMEMS sensor pre-LVAD surgery. The daily hemodynamic readings were used to guide patient management, pre- and post LVAD surgery. The aim was to normalize and keep the mean pulmonary artery pressure (mPAP) normalized (≤25 mmHg). For this analysis, patients were divided into those with a normal mPAP at all the scheduled follow-up moments at 3, 6, and 9 months post-LVAD surgery and those with an elevated mPAP during at least one of the follow-up moments. QoL was assessed by the EQ-5D-5L, KCCQ and PHQ-9 questionnaires at baseline (pre-LVAD surgery) and 3, 6 and 9 months post-LVAD surgery. The median age was 60 [52–63] years, and 70% of patients were men. In the hemodynamic normalized patients, QoL improved significantly between pre-LVAD surgery and the post-LVAD surgery follow-up moments, while no significant improvement was observed in the non-hemodynamic normalized patients. An increase of 37 points on the overall summary score of the KCCQ (p=0.046) was observed in the hemodynamic normalized patients, compared to a 22 points increase in the non-hemodynamic normalized patients (p=0.655), similar improvements were observed for the clinical summary score of the KCCQ, the visual analog scale of the EQ-5D and in the PHQ-9. Additionally, a trend towards a bigger improvement in the QoL was observed in the hemodynamic normalized patients, compared to the non-hemodynamic optimized patients (Figure). Successful hemodynamic management of LVAD patients, guided by CardioMEMS improves the QoL during the first year post-LVAD surgery. Patients who were hemodynamically normalized had a better QoL, and a bigger improvement in QoL from baseline, compared with non-hemodynamically optimized LVAD patients. Figure 1. Absolute and paired change in A EQ-5D-5L index value; B EQ-5D-5L visual analog scale, C KCCQ clinical summary score, D KCCQ overall summary score, E PHQ-9 score from baseline to 9 months of follow-up according to hemodynamically optimized status Type of funding source: Public hospital(s). Main funding source(s): This work was supported by Abbott with an independent research grant, partially covering personnel costs. This study was investigator-initiated and was designed, conducted, interpreted and reported independently of the funder.
Journal Title: European Heart Journal
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!