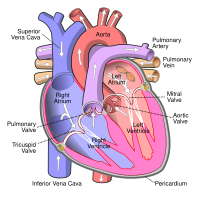
Photo from wikipedia
Mitral valve prolapse (MVP) is known to be associated with ventricular arrhythmias (VA), from symptomatic premature ventricular contractions (PVCs) to malignant ventricular tachycardia (VT) and sudden cardiac death (SCD). Previous… Click to show full abstract
Mitral valve prolapse (MVP) is known to be associated with ventricular arrhythmias (VA), from symptomatic premature ventricular contractions (PVCs) to malignant ventricular tachycardia (VT) and sudden cardiac death (SCD). Previous studies identified risk factors for VA in these patients such as young woman, bileaflet prolapse and inverted T-waves, but they included only specific cohort of patients who experienced SCD or who had only trivial or mild mitral regurgitation (MR). The prevalence of VA and their potential risk factors in a population of MVP patients with severe MR are unknown. The aim of our study was to describe the prevalence of VA in patients who underwent mitral valve surgery for moderate to severe MR due to MVP and to identify clinical, electrocardiographic and echocardiographic parameters associated with VA. 797 patients (65±12 years, 65% male) who underwent surgery for MVP were included from 2000 until 2018. The presence of VA was defined as symptomatic and frequent PVCs (Lown grade ≥2), non-sustained ventricular tachycardia (nsVT), VT or ventricular fibrillation (VF) documented before surgery and without an ischemic cause. The echocardiogram and electrocardiogram (ECG) prior to operation were used for the specific analysis. ECGs were checked for rhythm, conduction times, QRS morphology and inferior T-wave inversion. The origin of the PVCs was derived from a 12-lead ECG when available and divided in 5 groups; mitral annulus, papillary muscle (PM), left ventricle (LV, including outflow tract), right ventricle (including outflow tract) and other. By echocardiography, several parameters such as LV thickness and volumes, LV ejection fraction (EF), global longitudinal strain (GLS) and MR grade were obtained. A total of 99 (12%) patients showed VA; 70% (69/99) of the patients had symptomatic PVCs, 36% (36/99) had nsVT, 12% (12/99) VT and 3% (3/99) VF. 21 patients had more than one type of VA, of which the combination PVCs and nsVT was the most common (19/99, 19%). In addition, 6 patients experienced an out of hospital cardiac arrest of a non-ischemic cause. When comparing the clinical characteristics (Table), patients with VA were significantly younger (and with better renal function), more frequently diagnosed with Barlow's disease and experienced more palpitations as compared to patients without VA. The ECG analysis showed that patients with VA more often had inferior T-wave inversions and that the PVCs predominantly originated from the PM whereas in patients without VA the PVCs originated from different regions. Echocardiography showed that patients with VA had a thinner posterior wall, reduced LV EF and worse GLS; more severe MR was not associated with VA. In MVP patients with moderate to severe MR undergoing surgery, Barlow's disease, inferior T-wave inversions, thinner posterior wall and LV systolic dysfunction are associated with the presence and development of VA.
Journal Title: European Heart Journal
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!