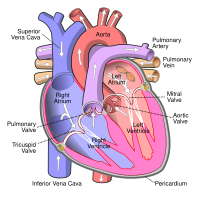
Photo from wikipedia
Accurate assessment of aortic annulus and left ventricular outflow tract (LVOT) anatomy is mandatory for appropriate device selection in order to achieve optimal deployment of transcatheter heart valves (THV). To… Click to show full abstract
Accurate assessment of aortic annulus and left ventricular outflow tract (LVOT) anatomy is mandatory for appropriate device selection in order to achieve optimal deployment of transcatheter heart valves (THV). To evaluate the impact of LVOT shape as determined by the sphericity index (ratio of long and short LVOT diameter) on THV hemodynamics. 1000 consecutive patients diagnosed with severe symptomatic aortic stenosis and undergoing TAVI between May 2008 and July2017 were analyzed. Assessment of aortic root dimensions including the LVOT was performed by contrast-enhanced multidetector computed tomography (MDCT) in all patients. The primary endpoint was 30-day device success as defined by the VARC-2 criteria. Secondary endpoints included all-cause mortality, cardiovascular mortality, permanent pacemaker implantation (PPI), and a 30-day combined early safety endpoint (all-cause mortality, all strokes, life threatening bleeding, acute kidney injury stage 2 or 3, CAD obstruction requiring intervention, major vascular complication, valve related dysfunction requiring repeat intervention). Patients were divided into 3 groups according to LVOT sphericity index (SI) quartiles. The three groups (low-SI: 0.4–0.63, n=250; mid-SI: 0.64–0.75, n=500; high-SI: 0.76–1.0, n=250) were well balanced in terms of baseline characteristics, except for gender distribution with more female patients in the low-SI group (36.8% vs. 49.0% vs. 60.0%; p=0.ehz748.05941). Assessment of calcification volume and Agatston score demonstrated significantly higher aortic valve and LVOT calcification in the high-SI group. The primary endpoint of device success after 30-days did not differ between the 3 groups (92.4% vs 91.9% vs. 87.9%; p=NS). However, moderate or severe paravalvular regurgitation (PAR) occurred significantly more often in the high-SI as compared to the other groups (4.1% vs. 5.2% vs. 10.6%; p=0.004 for low-SI vs. high-SI). In contrast, PPI rates, the early safety endpoint at 30 days, and all-cause mortality at 1 year did not differ between the groups. In the high-SI group implantation of a BE valve was associated with a significantly higher rate of device success as compared to SE valves (93.8% vs. 82.2%, p=0.007). This difference was driven by a higher rate of moderate or severe PAR (6.9% vs. 15.3%, p=0.007) in patients treated with SE valves. Moreover, patients in the high-SI group receiving a SE valve required more often a PPI than those treated with a BE valve (26.2% vs 13.3%, p=0.012). There was no difference between the THV types in the other SI groups in terms of primary and secondary endpoints. A more circular LVOT is associated with higher aortic valve and LVOT calcification. Implantation of a SE THV results in higher rates of moderate or severe PAR and persistent conduction disorder requiring PPI in such patients.
Journal Title: European Heart Journal
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!