Photo from wikipedia
Can machine learning (ML) predict oocyte’s fertilization and blastocyst development potential based on morphological features extracted from single static images? AI accurately predicted 70.4% of fertilization and 60.4% of blastocyst… Click to show full abstract
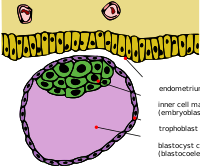
Can machine learning (ML) predict oocyte’s fertilization and blastocyst development potential based on morphological features extracted from single static images? AI accurately predicted 70.4% of fertilization and 60.4% of blastocyst development outcomes from a database of 1000 oocytes. Some morphological features of the oocyte have been associated with IVF-related outcomes, such as size, shape, and coloration of zona pellucida, polar body, perivitelline space, cytoplasm, and the meiotic spindle. Based on these characteristics, clinics might discard the low-quality oocytes according to a subjective assessment. AI-based algorithms could reduce the subjectivity and improve prediction on IVF outcomes such as successful fertilization and blastocyst development. Non-intervention study based on a cohort of 1000 oocytes’ micrographs collected between January 2019 and December 2020 from two IVF clinics. The inclusion criteria were known fertilization and blastocyst development outcome, and patient’s age between 25 and 45 years old undergoing IVF/ICSI treatment. Different features were considered for this study including metadata from oocyte’s (e.g. age, source), as well as manually extracted morphological features from the oocytes’ images (e.g. diameters, shape, granularity, presence/absence of spindle). We trained three machine-learning (ML) classifiers (i.e. Support Vector Machine, logistic regression, and neural networks) to predict successful fertilization and blastocyst development. For the training process we used a 10-fold cross validation approach to assess the model’s generalization capabilities. Besides we tested the statistical difference of each feature among groups (i.e. fertilized and no fertilized) using a two sided Student’s t-test for numerical and Z-test for categorial features (significance of p < 0.01). Our database showed 68.2% of successful fertilization and 34.8% of blastocyst formation. To balance the training data (50% per training class), we aleatory selected 318 and 348 samples per branch of successful/unsuccessful fertilization and blastocyst formation, respectively. From all ML classifiers, the neural network obtained the best results with an accuracy of 0.70 (AUC of 0.74) for predicting fertilization; and an accuracy of 0.60 (AUC of 0.62), for predicting blastocyst formation. We found that spherical shape, presence of meiotic spindle, clear coloration, larger oocyte diameter, thicker zona pellucida, and smaller vacuoles are statistically associated with both successful outcomes. As expected, we also found a strong association between age groups and outcome. The younger group (<35 years) demonstrated to have a larger proportion of successful fertilization compared to the rest of the age groups (36–37, 38–39, 40–42, >42). For the blastocyst formation we observed a similar association. It is relevant to note that all cycles were performed under a mini-IVF protocol. Oocytes extracted through conventional stimulation might show the same associations, but it would need further testing. Wider implications of the findings: The present study revealed that our system can predict fertilization success and blastocyst development potential based on metadata and morphometric features extracted from single digital micrographs of oocytes, offering a novel, adaptable and robust integration into clinical practice. CONBIOETICA–09-CEI–001–2017–0131
Journal Title: Human Reproduction
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!