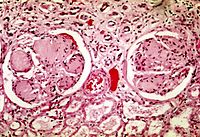
Photo from wikipedia
To measure and compare the risks of end-stage renal diseases (ESRD), cardiovascular diseases (CVD), all-cause mortality between obese type 2 diabetes mellitus (T2DM) patients with and without bariatric surgery. A… Click to show full abstract
To measure and compare the risks of end-stage renal diseases (ESRD), cardiovascular diseases (CVD), all-cause mortality between obese type 2 diabetes mellitus (T2DM) patients with and without bariatric surgery. A retrospective population-based cohort of 1,690 obese T2DM patients who were free of ESRD and CVD were assembled based on 2006-2017 Hospital Authority database. One-to-five propensity-score matching was used to balance baseline covariates between patients in bariatric surgery and control groups. Incidence rates (IR) of stage 4/5 chronic renal diseases, ESRD, CVD and all-cause mortality events for two groups were calculated. Hazard ratios (HR) for stage 4/5 chronic renal diseases, ESRD, CVD events were assessed using Cox proportional hazard models. Changes in estimated glomerular filtration rate (eGFR), and urine albumin-creatinine ratio (UACR) were measured up to 60 months. Over a mean follow-up period of 34 months with 863 person-years, cumulative incidences of mortality, stage 4/5 chronic kidney diseases, ESRD and CVD for surgical patients were 0, 0.050, 0.017, and 0.036, respectively. Surgical patients had reduced IR of all-cause mortality, stage 4/5 chronic kidney diseases, ESRD and CVD (IR=0, 1.784, 0.587 and 1.321 per 100 person-years, respectively) than control patients (IR=1.954, 2.028, 0.914 and 2.814 per 100 person-years, respectively). Surgery group had a significant reduction in risk of CVD events (HR=0.464, P=0.015), and no occurrence of mortality events. However, the IR of stage 4/5 chronic kidney diseases and ESRD of the two groups were not significantly different. Surgical patients had significantly higher eGFR within 12 months, and had significantly lower until 48 months. Among obese T2DM patients, bariatric surgery lowered the risk of CVD and mortality, and was beneficial towards the kidney outcomes of eGFR up to 36 months.
Journal Title: Nephrology Dialysis Transplantation
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!