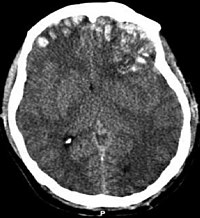
Photo from wikipedia
www.ccmjournal.org Critical Care Medicine • Volume 46 • Number 1 (Supplement) Learning Objectives: Intracranial pressure (ICP) monitoring and treatment to prevent raised ICP are common in neurocritical care. Largely based… Click to show full abstract
www.ccmjournal.org Critical Care Medicine • Volume 46 • Number 1 (Supplement) Learning Objectives: Intracranial pressure (ICP) monitoring and treatment to prevent raised ICP are common in neurocritical care. Largely based on adult traumatic brain injury (TBI) studies, a threshold of 20 mmHg is widely used, however a treatment target has not been well established in pediatrics. The objective of this study was to identify ICP thresholds that predict in-hospital mortality in children. Methods: An IRB-approved query of the electronic health record from a pediatric tertiary care center was performed to collect every recorded ICP measurement from 2012–16. Patient sex, age, admission diagnosis, date of death, and serial ICP measurements were obtained. Pairwise comparisons were performed using Mann-Whitney, and Youden’s index cut-points were generated from receiver operating characteristic (ROC) curves. Results: A total of 62,882 ICP measurements were obtained from 259 patients (8.4 ± 5.8 yrs, 63% male; mean ± SD). Associated mortality rates for select admission diagnoses include TBI (16%, n = 85), brain tumor with or without hydrocephalus (2%, n = 45), ICP monitoring to rule out intracranial hypertension (0%, n = 34), spontaneous intracranial hemorrhage (12%, n = 25), and shunt infection/malfunction (9.5%, n = 21), with a total in-hospital mortality of 10.8%. Mean and Peak ICP were higher among patients who died (19.1 [8.7–46.7] vs 12.0 [10.3–14.1] mmHg, p < 0.001 and 57.5 [33–75] vs 38 [27–55] mmHg, p = 0.001, respectively; median [IQR]). ROC analysis for the prediction of mortality using mean ICP had an area under the curve (AUC) 0.74, 95% CI (0.61, 0.87), cut-point ≥14.6 mmHg and peak ICP had an AUC 0.69, 95% CI (0.56, 0.81), cut-point ≥48.5 mmHg. Subgroup analysis of patients with TBI (mortality rate 16%) found mean ICP predicted mortality with an AUC of 0.69, 95% CI (0.46, 0.91), cut-point ≥17.5 mmHg, while peak ICP predicted mortality with an AUC of 0.62, 95% CI (0.42, 0.82), cut-point ≥48.5 mmHg. Conclusions: ICP thresholds were identified for the prediction of in-hospital mortality among pediatric neurocritical care and TBI patients. Further study is necessary to determine the impact of isolated vs. sustained elevations in ICP above described thresholds and the impact of age, mechanisms and patterns of injury, with the goal of developing precision-based ICP targets for pediatric neurocritical care patients.
Journal Title: Critical Care Medicine
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!