Photo from wikipedia
Learning Objectives: Ketamine is recommended as an induction medication for pediatric tracheal intubation (TI) with septic shock. However, ketamine is known as a direct myocardial depressant, and adult studies show… Click to show full abstract
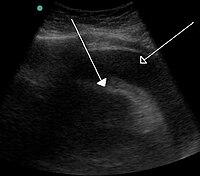
Learning Objectives: Ketamine is recommended as an induction medication for pediatric tracheal intubation (TI) with septic shock. However, ketamine is known as a direct myocardial depressant, and adult studies show ketamine often causes hypotension. We hypothesized that ketamine use for TI in the pediatric intensive care unit (PICU) is associated with fewer hemodynamic TI-associated events (TIAEs) compared to induction using other agents, and this association is similar in children with and without preexisting shock. Methods: We designed a retrospective cohort study to evaluate the occurence of hemodynamic TIAEs associated with the use of ketamine as an induction agent for TI in pediatric patients, both with and without septic shock, utilizing a multicenter pediatric airway quality improvement database (NEAR4KIDS) from January 2013 to June 2017. All children less than 18 years with initial TI in the PICU were included. We defined our outcome of hemodynamic TIAEs as dysrhythmia (including sinus bradycardia), hypotension, and cardiac arrest. Our exposure of interest was ketamine use. Stratified analysis among children with shock and without shock as TI indication was performed, and effect heterogeneity was assessed by the Mantel-Haenszel test. Multivariable logistic regression was used for effect size, accounting for factors associated with ketamine use. Results: Ketamine was used in 3436 (32%) of 10,750 TIs. Ketamine was more commonly used during shock, in respiratory failure, and for procedural indications. Univariate analysis demonstrated that ketamine use was associated with a lower rate of hemodynamic TIAEs when used for induction during TI (with shock: OR 0.81 [95% CI 0.58–1.12]; without shock: OR 0.72 [95% CI 0.57–0.90]). The OR for all patients who received ketamine was 0.74 (0.62–0.90); p=0.002. After adjusting for factors associated with ketamine use, we found that the use of ketamine continued to be significantly associated with a lower occurrence of hemodynamic TIAEs: OR 0.74 (95% CI 0.58–0.95); p=0.019. Conclusions: Ketamine use during induction is favorable in reducing hemodynamic TIAEs in children without preexisting shock and all children combined. Learning Objectives: Evaluation of fluid status is essential in a critically ill patient. In hypovolemic states, central venous pressure (CVP) is used to guide fluid management, yet has shown poor relationship to intravascular volume and is potentially inaccurate in predicting hemodynamic response to fluid challenge. Methods for assessment of fluid overload (FO) include fluid balance and change in weight over hospital course, yet both are subject to error and may be impractical in a mechanically ventilated child. Adult studies have shown assessment of the IVC by bedside ultrasound (BUS) in patients on mechanically ventilated patients has good correlation with fluid status (FS) and fluid responsiveness (FR). IVC distensibility index (IVCdi) over 18% and IVC/Aorta ratio (IVC:Ao) less than 0.8 are suggestive of FR. It is unknown how sonographic assessment of the IVC in mechanically ventilated children correlates with CVP, % FO and provider perception of FS. Methods: This was a prospective, observational study in ventilated children admitted to the pediatric intensive care unit with a CVP reading. Patients had a BUS of their IVC in the sagittal view and IVC and aorta in the transverse view. IVCdi and IVC:Ao were measured. Clinical data including CVP, fluid balance, weight and independent provider perception of FS (hypovolemic, euvolemic or hypervolemic) were recorded. Results: We have enrolled 44 patients. %FO by weight trends towards a significant correlation with IVC:Ao (p=0.053) and IVCdi (p=0.064) but had no correlation with CVP value or fluid balance. When FS is divided categorically by CVP< 8 (hypovolemia), CVP 8–12 (euvolemia) and CVP>12 (hypervolemia), IVCdi (p=0.009) is different between the groups. CVP does not correlate with %FO by weight (p=0.943) or balance (p=0.834). When using FR cutoffs of 18% for IVCdi and 0.8 for IVC:Ao, neither CVP, %FO or perception of FS is different in patients defined as FR. Conclusions: With additional enrollment, we expect to find IVCdi by BUS will correlate with %FO by weight and can be used for noninvasive, reliable assessment of FO. Similarly, IVCdi greater than 18% may identify patients who have CVP<8 and may respond to fluid administration. This may provide invaluable information for patients who do not have the ability to monitor CVP through an invasive line.
Journal Title: Critical Care Medicine
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!