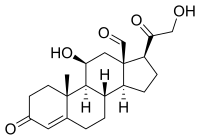
Photo from wikipedia
Objective: To assess the association between serum parathyroid hormone (PTH) or vitamin D serum levels with blood pressure, aldosterone-to-renin ratio, and target organ damage in a series of hypertensive patients.… Click to show full abstract
Objective: To assess the association between serum parathyroid hormone (PTH) or vitamin D serum levels with blood pressure, aldosterone-to-renin ratio, and target organ damage in a series of hypertensive patients. Design and method: Observational cross-sectional study of hypertensive patients who undergone 24-hour ambulatory blood pressure monitoring (24-h ABPM), in whom plasma aldosterone, plasma aldosterone-to-renin ratio, PTH and 25-OH D serum levels were available. Blood pressure (BP) was measured by 24-hour ABPM. BP was assessed as average real variability. Renin-angiotensin-aldosterone axis status was assessed through plasma aldosterone levels and aldosterone-to-renin ratio. Electrocardiography, echocardiography and urine albumin-to-creatinine ratio were used to evaluate left ventricular hypertrophy and renal damage, respectively. Patients with primary hyperparathyroidism were excluded. Results: We enrolled 170 consecutive patients (median age [IQR] -year), 52 [42–64]; 48.2%, female). In comparison with patients with normal PTH serum levels (<88 pg/ml), those with high PTH serum levels (>88 pg/ml) showed a significantly increase in plasma aldosterone-to-renin ratio [mean ± SD] (37.8 ± 46.6 vs. 20.7 ± 27.0; p = 0.032), and nocturnal pulse pressure (56.3 ± 17.9 vs. 50.6 ± 13.1 mm Hg; p = 0.029). Furthermore, when compared with patients in the PTH 1st quartile, those in the 4th PTH quartile showed significantly higher nocturnal systolic BP (129.5 ± 25.6 vs. 119.9 ± 14.4 mm Hg; p = 0.038), plasma aldosterone (204.9 ± 128.4 vs. 153.8 ± 88.7 pg/ml; p = 0.037), plasma aldosterone-to-renin ratio (36.4 ± 45.8 vs. 18.9 ± 24.5; p = 0.033), and nocturnal mean BP variability (8.9 ± 4.4 vs. 7.1 ± 1.7 mm Hg; p = 0.016). Differences in aldosterone-to-renin ratio and nocturnal mean BP variability remained significant after adjusting by age, gender, renal function and ACE/ARB therapy in multivariate analysis. No such differences were observed in patients with vitamin D deficiency (25-OH D < 20 ng/ml), when compared with patients with normal vitamin D serum levels. Conclusions: High PTH, but not low 25-OH D serum levels associate with increased aldosterone-to renin ratio and elevated nocturnal mean blood pressure variability. Our results might explain, in part, the lack of consistent clinical benefit of vitamin D supplementation on high blood pressure and cardiovascular risk. We suggest that serum PTH status should be considered in trials searching for cardiovascular benefits from vitamin D supplementation in patients with hypovitaminosis D.
Journal Title: Journal of Hypertension
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!