Photo from wikipedia
Background: Antibody-mediated rejection (ABMR) is the major cause of kidney transplant failure, which requires donor-specific antibodies (DSA) for a definitive diagnosis based on Banff 2013. However, lack information about donor’s… Click to show full abstract
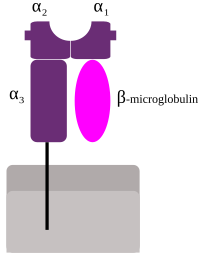
Background: Antibody-mediated rejection (ABMR) is the major cause of kidney transplant failure, which requires donor-specific antibodies (DSA) for a definitive diagnosis based on Banff 2013. However, lack information about donor’s HLA genotypes is often encountered in clinic practice, which affects the determination of HLA-related DSA. Donor-derived cell-free DNA (ddcfDNA) in urine from graft-cell apoptosis and necrosis, which contains the genomic information of the donor. Compared with other molecular methods (i.e. SBT, SSP, SSOP), NGS is a high-throughput sequencing, which has an advantage in typing HLA homozygous loci, and provides more precise results than serological for identifying donor’s HLA. This study intends to establish a non-invasive method for donor’s HLA typing in kidney transplant patients by target capture sequencing. Methods: We developed a method based on target region (HLA-A, -B, -C, DRB1, -DQB1, -DPB1) capture sequencing (to simultaneously examine blood and urine of kidney transplant patients. cfDNA is extracted from urine and gDNA from blood. The HLA typing data from cfDNA is considered to be the combination of both recipient and donor HLA phenotypes, and the HLA typing data of gDNA is considered to be only from the recipient. Donor’s HLA could thus be identified from cfDNA result and the recipient’s HLA data. Results: In the analysis of capture sequencing results, all target HLA sites of blood sample (HLA-A, -B, -C, -DRB1, -DQB1, -DPB1) were successfully sequenced and had a higher resolution (4-digits) for HLA typing from 5 patients. 60 alleles (5*6 loci*2 diploid) were successfully detected, including 3 pairs of homozygous loci (A*24:02, DPB1*05:01, DQB1*03:01) and 27 pairs (90%) of heterozygous loci. In comparison with HLA genotypes of recipient blood samples by PCR-SSO, only one allele (B*62) was inconsistent with our results (B*15:01). In urine HLA typing results, 77 HLA genotypes were detected (A=12, B=14, C=11, DPB1=15, DQB1=13, DRB=12), of which 41 HLA genotypes were consistent with the recipient’s HLA genotype, so the remaining 36 HLA genotypes were considered to be from the donor. Among the alleles of donor’s HLA genotype, HLA-I accounted for 47.2%, and HLA-II accounted for 52.8%. The results showed that 80% of the donor’s HLA genotypes in the urine were consistent with donor HLA typing results by PCR-SSO. Conclusions: This urine-based method offers a reliable non-invasive method for the identification of donor’s HLA genotype in kidney transplant recipients with unknown donor HLA phenotype. P-2.04
Journal Title: Transplantation
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!