Anesthesiology, V 126 • No 1 1 January 2017 A s of 2012, angiotensinconverting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) were used by approximately 18% of adults… Click to show full abstract
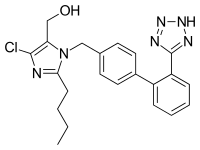
Anesthesiology, V 126 • No 1 1 January 2017 A s of 2012, angiotensinconverting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) were used by approximately 18% of adults in the United states.1 In the Veterans Affairs medical system, a population with a high proportion of patients with cardiovascular disease and strong centralized efforts at cardiovascular guideline compliance, as many as 43% of patients present for major surgery on either of these agents.2 In contrast to current guidelines3 according Class I recommendation for continuation of β-blockers on the day of surgery (and after) in patients without contraindications, considerable controversy exists regarding administration of ACEIs/ARBs. In this issue of A nEsthEsIology, Roshanov et al.4 present a sophisticated observational analysis of the associations of ACEI/ARB administration versus withholding of the dose within 24 h before noncardiac surgery in the large multinational, prospective observational cohort (Vascular events In noncardiac surgery patIents cohort evaluation [VIsIon]). Their findings suggest that administration on the day of surgery is hazardous, a finding that may perhaps finally lead to the large randomized clinical trial needed to definitively answer this chronic vexing issue. Clinical investigation of the consequences of preoperative administration of ACEIs had first been reported in the cardiac and vascular surgical settings in the early 1990s in small randomized and observational cohort studies from two centers in France. one center focused on a higher observed incidence of hypotension on induction with their preoperative administration and the need for potent vasoconstrictors for its treatment.5,6 The other suggested that although simple volume infusion was adequate to prevent hypotension, during aortic cross-clamping (in vascular surgery) where the glomerular filtration rate was measured, a significant decrease was noted in some patients.7 over the ensuing years to the present, ARBs were introduced; larger cohort analyses have reported conflicting results with regard to the incidence of drug-induced hypotension and its relation to adverse outcomes including mortality, myocardial infarction (MI), and of more recent interest, renal failure and atrial fibrillation (the latter in cardiac surgery only).8,9 Attempts to systematically analyze the literature have been inconclusive due to the lack of high-quality randomized trials, small sample sizes, and variable outcomes reported in observational analyses.10–12 Despite concerns over the safety of the immediate preoperative or any perioperative administration of these commonly prescribed medications, with strong guideline-based evidence of their benefits in patients with hypertension, post-MI, congestive heart failure, diabetes, and chronic renal disease in the nonoperative setting,13 many clinicians are reticent to withhold them during the stressful perioperative period. Current noncardiac and coronary artery bypass graft surgery guidelines support their continuation or transient discontinuation (with reinstitution later in the perioperative period) but make no Class I or Class III (harm) recommendations.3,14,15 Preoperative Administration of Angiotensin-converting Enzyme Inhibitors or Angiotensin II Receptor Blockers