Photo from wikipedia
Abstract Background: Percutaneous coronary intervention with the new generation drug eluting stents (DES) is 1 among the revascularization procedures required to treat patients with coronary artery disease (CAD). Since late… Click to show full abstract
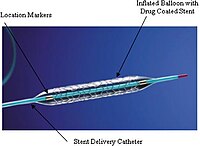
Abstract Background: Percutaneous coronary intervention with the new generation drug eluting stents (DES) is 1 among the revascularization procedures required to treat patients with coronary artery disease (CAD). Since late stent thrombosis and silent myocardial infarction are highly associated with type 2 diabetes mellitus (T2DM), an analysis comparing the newer generation DES in this specific subgroup of patients would be scientifically relevant. In this analysis, we aimed to systematically compare the cardiovascular outcomes observed with the ultrathin bioresorbable polymer sirolimus eluting stents (SES) versus thin, durable polymer everolimus eluting stents (EES) following percutaneous coronary intervention in patients with T2DM. Methods: Through online databases, relevant studies comparing ultrathin bioresorbable polymer SES versus the durable polymer EES were carefully searched. The cardiovascular outcomes were assessed during a follow-up time period of 1 year and more than 1 year (1–5 years) respectively. This meta-analysis was carried out by the latest version of the RevMan software. Following analysis, the results were represented by odds ratios (OR) with 95% confidence intervals (CI). Results: A total number of 1967 patients with T2DM were included in this analysis. During a 1 year follow-up time period, target lesion failure (TLF) (OR: 0.59, 95% CI: 0.34–1.02; P = .06, target vessel revascularization (TVR) (OR: 0.97, 95% CI: 0.55–1.70; P = .91) and target lesion revascularization (TLR) (OR: 0.91, 95% CI: 0.44–1.87; P = .79) were similarly observed with ultrathin bioresorbable polymer SES versus the thin, durable polymer EES in these patients with T2DM. Other cardiovascular outcomes including myocardial infarction (MI), major adverse cardiac events, all-cause mortality (OR: 0.72, 95% CI: 0.37–1.40; P = .34), cardiac death and stent thrombosis (OR: 0.85, 95% CI: 0.45–1.62; P = .63) were also similarly observed with these 2 types of new stents. During a follow-up time period above 1 year (1–5 years), still no significant difference was observed in TLF, TVR, TLR, major adverse cardiac events, MI, all-cause mortality, cardiac death and stent thrombosis (OR: 0.62, 95% CI: 0.33–1.16; P = .14). Conclusions: The ultrathin bioresorbable polymer SES were similar to the durable polymer EES in these patients with T2DM. These 2 types of new generation stents were comparable in terms of cardiovascular outcomes. Hence, they might be recommended in patients with T2DM. Upcoming trials should be able to confirm this hypothesis.
Journal Title: Medicine
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!