Photo from wikipedia
If there is anything the last few decades have taught us, it is that researchers must properly conduct studies on vitamin supplements before they can make health claims. In a… Click to show full abstract
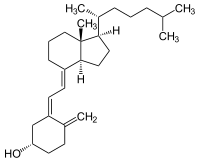
If there is anything the last few decades have taught us, it is that researchers must properly conduct studies on vitamin supplements before they can make health claims. In a recent paper by Lai et al. (2022), the authors state, “vitamin D supplementation worsens Alzheimer's progression” without sufficient evidence to support these conclusions. While certain findings are scientifically interesting, readers must understand substantial limitations in the approach and methodology utilized in the paper limit conclusions one can make about the role of vitamin D in brain health and Alzheimer's disease (AD). Before proceeding further, it is important for readers to understand that there are three different forms of vitamin D pertinent to this discussion. Cholecalciferol is the form of vitamin D3 synthesized in the skin upon exposure to UVB rays that typically come from sunlight. It is also the form found in dietary supplements. The liver converts cholecalciferol to calcidiol (25hydroxyvitamin D3), the circulating form used by clinicians to determine vitamin D status. Certain cells in the body will then convert calcidiol to calcitriol (1,25dihydroxyvitamin D3), the “active” form of vitamin D in the body (Bikle, 2000). Calcitriol is a highaffinity, potent ligand for the vitamin D receptor (VDR) and regulates most VDRdependent gene transcription. The body only produces calcitriol under certain physiological conditions, including low serum calcium levels or immune activation, and tightly controls its synthesis and catabolism to limit its physiological effects. On the other hand, cholecalciferol and calcidiol are considered inactive forms of vitamin D3, as they are lowaffinity ligands for VDR (Bikle, 2000). Because these three forms are not functionally or physiologically equivalent, referring to them all as “vitamin D” creates a great deal of confusion, especially since cholecalciferol is found in vitamin D supplements or fortified foods and beverages, but calcitriol is appropriately classified as a drug (Vieth, 2020). The study by Lai et al. begins with data from neuronal cell culture. Here, the authors demonstrate that treatment with both calcidiol and calcitriol increases apoptosis and autophagy in undifferentiated SHSY5Y cells upon exposure to Aβ42. SHSY5Y is a neuroblastoma cell line typically used in experiments after differentiation into a homogeneous, more mature neuronlike cell, making them useful for AD research (Agholme et al., 2019). Prior reports show calcitriol protects differentiated SHSY5Y cells against Aβ(1– 42) peptide cytotoxicity (Vieth, 2020), although others have reported protection of undifferentiated SHSY5Y cells from Aβ(25– 35) toxicity upon treatment with calcitriol (Lin, Chang, et al., 2020). While the study by Lai et al. reports contradictory findings, the authors do not discuss them in the context of the greater literature base, so it is unclear what could have explained these divergent responses. Encouraged by their cell culture findings, the authors performed a vitamin D (cholecalciferol) feeding study in an APP/PS1 transgenic mouse model. This model, like most murine models for AD, recapitulates a rare form of AD that mirrors limited aspects of human AD pathology. It does not represent normal cognitive decline or even commonly seen forms of AD in humans. These animals also have difficulties maintaining vitamin D status, as evidenced by lower serum calcidiol levels compared to wildtype controls when maintained on a 600 IU/kg cholecalciferol diet. Feeding the mice a high vitamin D diet containing 8044 IU/kg cholecalciferol starting at the age of 4.5 months restored serum calcidiol levels. However, after 3 months of supplementation, the authors observed “more severe Aβ plaque deposits and reactive gliosis in the hippocampus compared to the controls,” an increased expression of prodegenerative factors in the
Journal Title: Aging Cell
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!