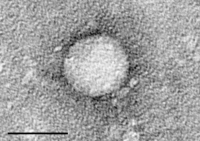
Photo from wikipedia
Fibrosing cholestatic hepatitis (FCH) posttransplantation can lead to graft failure and death. In the era of direct acting antiviral therapy (DAA), several studies have demonstrated the efficacy and safety of… Click to show full abstract
Fibrosing cholestatic hepatitis (FCH) posttransplantation can lead to graft failure and death. In the era of direct acting antiviral therapy (DAA), several studies have demonstrated the efficacy and safety of transplanting hepatitis C virus (HCV)–positive allografts into HCV‐negative recipients. In this case series, we present two cases of HCV‐negative recipients who underwent kidney transplantation from viremic donors and developed FCH. Both patients presented after transplant with abnormal liver function tests and HCV viral loads of greater than 100 000 000 IU/mL. FCH was diagnosed by histology and/or clinical data. Both patients were started on DAA therapy within 24 hours of admission with improvement in LFTs. One patient has undetectable HCV 12 weeks after completing treatment and the other patient has undetectable HCV after completing DAA treatment. The introduction of DAAs has changed the landscape of solid organ transplantation with the potential to expand the donor pool and increase access to organs. While HCV viremic organs have tremendous potential to increase access to a scarce resource, FCH is a potentially fatal complication and therefore clinicians must maintain a high index of suspicion for this unique complication.
Journal Title: American Journal of Transplantation
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!