Photo from wikipedia
Azoospermia can be diagnosed in about 10%–15% of the infertile male population. To overcome the problem of failure to produce spermatozoa in the ejaculate in patients with nonobstructive azoospermia (NOA),… Click to show full abstract
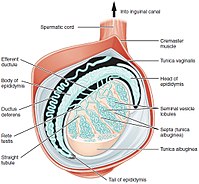
Azoospermia can be diagnosed in about 10%–15% of the infertile male population. To overcome the problem of failure to produce spermatozoa in the ejaculate in patients with nonobstructive azoospermia (NOA), testicular sperm extraction (TESE) may be performed to find the focal area of spermatogenesis. A 47‐year‐old man with NOA presented for treatment of secondary couple infertility. The patient underwent a first TESE 7 years earlier with cryopreservation, and an intracytoplasmic sperm injection–embryo transfer ended in a term pregnancy. He reported a history of repeated testicular traumas. At the present time, a complete medical workup was carried out, including clinical history, general and genital physical examination, scrotal and transrectal ultrasounds. Hormone measurements showed follicle‐stimulating hormone level of 42.7 IU/L, luteinising hormone of 11.4 IU/L, total testosterone of 2.6 ng/ml and right and left testicular volume, respectively, of 4 and 3.9 ml. He underwent a second TESE, with successful sperm retrieval and cryopreservation. The histological pattern was hypospermatogenesis. In cases of extreme testicular impairment, although in the presence of very high follicle‐stimulating hormone value and small testicular volume, estimating poor sperm recovery potential, the integration of clinical and anamnestic data, could help the surgeon to practise the more appropriate method of treatment.
Journal Title: Andrologia
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!