Photo from wikipedia
A 52-year-old female was found to have an intra-abdominal mass following a computed tomography scan of the abdomen and pelvis for an unrelated presentation. The patient’s past medical history included… Click to show full abstract
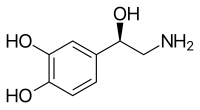
A 52-year-old female was found to have an intra-abdominal mass following a computed tomography scan of the abdomen and pelvis for an unrelated presentation. The patient’s past medical history included hypertension, managed with telmisartan. The mass, measuring 33 × 42 mm axially and 58 mm craniocaudally, lay anterior to the abdominal aorta and extended laterally between the aorta and inferior vena cava. The lesion arose inferior to the superior mesenteric artery, compressing the left renal vein (Fig. 1). The mass was initially thought to represent lymphadenopathy, prompting a fluorodeoxyglucose positron emission tomography scan, which demonstrated intense focal uptake (SUV max 54.9). Core biopsy favoured a paraganglioma or low-grade neuroendocrine tumour. Serum analysis detected elevated plasma 3-methoxytyramine (520 pmol/L, range <181 pmol/L) and chromogranin-A (7.5 nmol/L, range <3 nmol/L). Remaining biochemistry, including plasma normetanephrine (510 pmol/L, range <830 pmol/L), metanephrine (270 pmol/L, range <447 pmol/L), adrenaline (<0.3 nmol/L, range <1.5 nmol/L), noradrenaline (2.1 nmol/L, range 0.1–6.3 nmol/L), 24-h urinary noradrenaline (284 nmol/day, range 100–420 nmol/day), adrenaline (<3 nmol/day, range 0–80 nmol/day) and serotonin (0.67 μmol/day, range 0.10–0.80 μmol/day), was normal. Supine blood sampling occurred following overnight fasting and low catecholamine diet 24 h prior to urinalysis. The case was discussed at a multidisciplinary meeting, and preoperative advice was obtained from an endocrinologist. Given that she was asymptomatic and denied vasogenic symptoms, it was advised that no preoperative adrenoreceptor blockade was required. Iodine-123 metaiodobenzlyguanidine scintigraphy and gallium-68 DOTATATE positron emission tomography (Fig. 1) scans were performed for staging and to further support either histopathological diagnosis. These demonstrated increased uptake in the para-aortic mass, consistent with expression of noradrenaline transporters and somatostatin receptors. This patient’s catecholamine profile may be due to the tumour lacking dopamine beta-hydroxylase, leading to impaired synthesis of noradrenaline and adrenaline but increased dopamine production. Previous studies have shown that the noradrenaline transporter is able to transport dopamine in addition to noradrenaline. Intraoperatively, a large, gourd-shaped mass, lying anterior to the abdominal aorta and inferior vena cava, was found. The left renal vein was tented by the tumour and was divided to facilitate access (Fig. 2). The tumour was dissected free from surrounding structures and removed with the capsule intact. The operation proceeded without immediate complications, and there was no haemodynamic instability during tumour manipulation or removal. The patient recovered well and was discharged home 6 days following surgery. Macroscopic examination demonstrated a nodular, brown mass, measuring 80 × 40 × 40 mm and weighing 51 g with a large, central haemorrhagic cavity. The tumour demonstrated moderate cellularity in a Zellballen pattern without comedo necrosis (Fig. 3). Histopathological examination and immunohistochemical testing were consistent with a moderately differentiated paraganglioma (GAPP score = 3), demonstrating normal, positive staining of succinate dehydrogenase (SDH) subunits A and B. Post-operative biochemical evaluation demonstrated normalization of 3-methoxytyramine (5 pmol/L). Paragangliomas are rare, extra-adrenal, chromaffin cell tumours, histologically similar to pheochromocytomas. The estimated incidence is less than three per million. Tumours may occur at any sympathetic or parasympathetic extra-adrenal paraganglia, most commonly the sympathetic trunk, bladder wall and organ of Zuckerkandl. They may be classified as functional or non-functional. Functional tumours secrete catecholamines, often causing the typical symptoms of episodic hypertension, tachycardia, diaphoresis and palpitations. The vast majority of functional tumours secrete adrenaline and/or noradrenaline; tumours secreting dopamine alone are very rare. Paragangliomas are commonly associated with various genetic mutations and syndromes, including SDHA, SDHB, SDHC, SDHD, SDHAF2, MAX, TMEM127, HIF2α, KIF1β, IDH1, FH, EGLN1/PHD2, Von Hippel–Lindau syndrome (VHL mutation),
Journal Title: ANZ Journal of Surgery
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!